What are the symptoms if a diabetic has poor kidney function?
summarize

Diabetic nephropathy is kidney damage caused by diabetes mellitus, which mainly consists of a glomerular filtration rate (GFR) of less than 60 ml/min/1.73 m2 or a urinary albumin/creatinine ratio (ACR) of more than 30 mg/g persisting for more than 3 months. Diabetic glomerulonephropathy is specifically defined as glomerulopathy caused by diabetes mellitus as confirmed by renal biopsy.
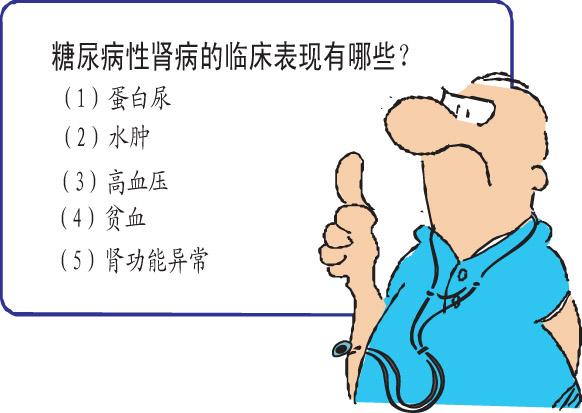
Diabetic nephropathy is one of the common complications in diabetic patients with a very high mortality rate, so early diagnosis and treatment is the most important thing that diabetic nephropathy patients should pay attention to. Kidney damage caused by diabetes mellitus is mainly diabetic glomerulosclerosis. Its clinical manifestations are mainly proteinuria, edema, hypertension and azotemia. In developed countries, diabetes is one of the main causes of end-stage renal disease.
What causes diabetic nephropathy?
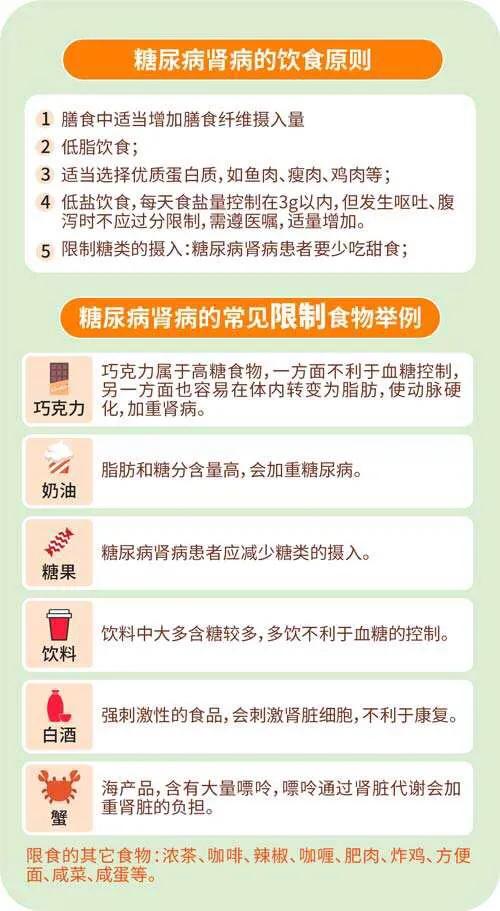
① high protein diet exacerbates the deterioration of diabetic nephropathy: diabetic patients due to strict restriction of carbohydrate intake, and high protein fiber food supply is the main, lose sight of the other, resulting in protein breakdown products and phosphorus overload and accumulation, and then exacerbate the pathological damage of kidney injury.
② the effect of hypertension: diabetic patients due to lipid metabolism disorders, atherosclerosis and many other reasons, combined with hypertension in a large number of patients, almost all of these patients can be seen in the urine micro-protein, indicating that renal damage is common.
(iii) Hyperglycemia: prolonged and excessive increase in blood glucose can lead to increase in capillary permeability, extravasation of plasma proteins, causing damage to capillary basement membrane, glomerulosclerosis and atrophy of renal tissue.
Diagnosis of diabetic nephropathy
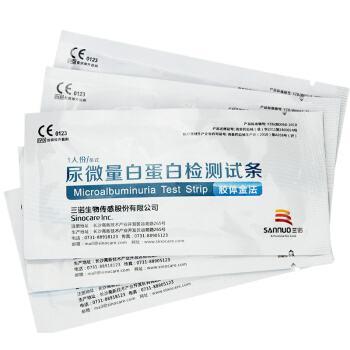
1、Measurement of microalbuminuria (UAE): UAE 20-200 micrograms per minute twice in six months, excluding other factors and heart failure, obstruction, etc. can be diagnosed as furunculosis nephropathy. Therefore, this is one of the diagnostic items of diabetic nephropathy.
2. Ultrasound and X-ray radiography: whether the kidneys are enlarged compared with normal people of the same age. Patients can detect kidney disease at an early stage by performing all examinations regularly. This diagnosis of diabetic nephropathy is more common.
3, excitation test: under a certain exercise load, normal people do not appear proteinuria, while early diabetic patients can appear proteinuria. Urine-N-acetate-B-glucosaminyltransferase (NAG), T-H glycoprotein, and urinary B2-microglobulin tests are all indicators for early diagnosis of diabetic nephropathy. Glomerular filtration rate was measured by 99Tin-DPTA. This also belongs to one of the diagnostic methods of diabetic nephropathy.
Manifestations and staging of diabetic nephropathy
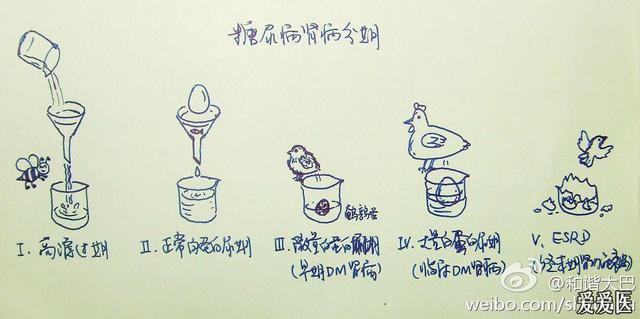
Type 1 diabetes mellitus renal damage is divided into 5 stages, progressing about one stage every 5 years, and this staging is now widely used by clinicians. In fact, type 2 diabetes mellitus renal damage process is similar to this, except that type 2 diabetes mellitus renal damage progresses faster than type 1 diabetes mellitus (about one stage every 3 to 4 years), which may be related to type 2 diabetes mellitus occurs in middle-aged and elderly people, the kidneys already have degenerative changes, and most of them are combined with hypertension and hyperlipidemia. The clinicopathologic manifestations of these 5 stages are briefly described as follows:
Stage Ⅰ: glomerular hyperfiltration stage
Characterized by increased glomerular filtration rate and increased renal volume.、This initial lesion is consistent with high blood glucose levels, but is reversible and can be restored with insulin therapy, but not necessarily to full normalization.
Stage II: stage of renal damage without clinical manifestations
In this phase, the urinary albumin excretion rate is normal but the glomeruli have developed structural changes. In this stage, the urinary albumin excretion rate (UAE) is normal (<20 μg/min or <30 mg/24h), and the group with increased UAE after exercise may recover after rest. In this stage, glomeruli have structural changes, the glomerular capillary basement membrane (GBM) is thickened and the tethered matrix is increased, the GFR is higher than normal and consistent with the blood glucose level, and the glycosylated hemoglobin of the patients with GFR>150mL/min is often >9.5%. patients with GFR>150mL/min and UAE>30μg/min are more likely to develop clinical diabetic nephropathy in the future. The blood pressure of patients with stage I and II diabetic kidney damage is mostly normal. Patients with stage I and II diabetic nephropathy have increased GFR and normal UAE, so stage II cannot be called diabetic nephropathy.
Stage III: Early diabetic nephropathy
The development of persistent microalbuminuria (persistent UAER of 20-200 μg/min or 30-300 mg/d) is the hallmark of this stage, but routine urinalysis remains negative for protein. The GFR is generally normal in this stage. Blood pressure often begins to rise. Pathologic examination of glomerular stroma widening and glomerular basement membrane (GBM) thickening is more obvious, and the walls of small arteries appear vitrified. It is generally believed that the renal lesions are irreversible from this stage onwards. The patient's blood pressure is mildly elevated and glomerular desertion begins to occur.
Stage IV: clinical diabetic nephropathy or overt diabetic nephropathy
This phase is characterized by massive albuminuria (>3.5 g per day), edema and hypertension. Edema is more severe in diabetic nephropathy and responds poorly to diuretics.
Stage V: i.e. end-stage renal failure
Once a diabetic patient develops clinical diabetic nephropathy with persistent urinary protein, renal filtration function declines progressively due to extensive thickening of the glomerular basement membrane, progressive narrowing of the glomerular capillary lumen and more glomerular desertion, leading to renal failure.
What are the symptoms of early diabetic nephropathy
1. Renal insufficiency. If diabetic patients once develop diabetic nephropathy, it will eventually lead to azotemia, uremia and other serious consequences.
2. Presence of retinopathy. Retinopathy is not a clinical manifestation of nephropathy, but it often coexists with diabetic nephropathy. It is even believed that diabetic nephropathy cannot exist without diabetic retinopathy.
3. Urine protein begins to appear. With the further development of the lesion, urinary protein gradually becomes persistent heavy proteinuria, if the urinary protein is more than 3 grams / day, this is more serious.
4. Swelling. Early diabetic nephropathy patients generally do not have edema, a small number of patients in the plasma protein before the decrease, there can be mild edema, when the 24-hour urine protein more than 3 grams, edema will appear. Patients with rapidly developing diabetic nephropathy will have obvious generalized swelling.
5, patients in the early stages of the disease will appear renal hypertrophy and glomerular hyperfiltration, proteinuria continued to increase, but this stage can be timely use of insulin to treat the disease, renal function can also be restored. The disease continues to develop, proteinuria excretion is abnormally high, from intermittent to persistent, the damage to the patient is more serious.
6. Increased urine output: normal people have a daily urine output of 1500-2000 milliliters. After suffering from diabetes mellitus, there are three phenomena, that is, eat more, drink more, urinate more, and the daily increase in urine volume exceeds that of normal people. This is because in the early glomerular filtration rate increases, urine volume also increases. This phenomenon can last for many years, and with further progression of the disease, the urine output can decrease a little, which is related to the decrease of glomerular filtration rate.
7, protein in the urine: this is diabetes damage to the glomerulus and other microvascular caused by a very important performance. The reason is that the glomerular filtration membrane pore enlargement and the original negative charge loss, as a result of plasma protein easily filtered out. Urine protein phenomenon early intermittent, some people use the excitation test, that is, let the diabetic patient exercise and then check the urine protein, if there is no proteinuria at rest, but appeared after the exercise, or after the exercise of urine protein further increase, called exercise proteinuria.
8, the emergence of nephrotic syndrome: if the patient's urine protein increase of more than 3 grams per day, accompanied by hypoproteinemia, obvious edema and hyperlipoproteinemia, is the manifestation of nephrotic syndrome. Renal experts believe that once the above phenomenon occurs in patients with sugar disease, the prognosis is sinister and will enter azotemia very quickly. At this time, the glomerular filtration rate is reduced, the urine protein is reduced instead, and the condition is more dangerous.
9, recurrent pyelonephritis: because diabetic patients have a large amount of glucose in the urine, bacteria can easily grow and multiply, and if there is urinary retention, the bacteria are more likely to grow; the patient's resistance is low, which makes pyelonephritis recurring, and thus it is difficult to be cured completely.
10. Nipple necrosis: this is a very serious situation. Renal vascular sclerosis, poor blood circulation, easy to cause tissue edema due to ischemia and hypoxia. Once infection occurs, inflammation is formed, and the treatment is not timely, tissue necrosis can occur rapidly, and the patient develops hematuria, pyuria, renal area colic, which can be further developed into septicemia, uremia, and the consequences are more dangerous.
What are the complications of severe diabetes?
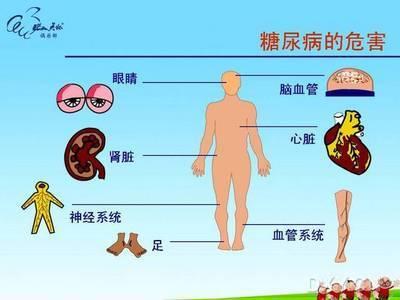
Complications of diabetes are divided into two main categories: acute complications and chronic complications. The details of these two types of diabetes complications are analyzed below:
1. Chronic complications.Regarding the complications of chronic diabetes, they are some of the more serious complications of diabetes.
①Renal: proteinuria, infection, renal failure
②Heart: coronary artery embolism, angina pectoris, heart failure, arrhythmia
③ Brain: cerebral congestion, cerebral embolism hemiplegia
④Eyes: cataract, glaucoma, retinopathy vision loss, blindness
⑤ Foot: numbness, ischemia, weakness, ulcers, amputations
2. Acute complications, acute complications are a common complication of diabetes.
① Hypoglycemic coma.
② Hyperglycemic coma (ketoacidosis, non-ketotic hyperosmolar coma)
③ Lactic acidosis
Daily Precautions for Diabetic Nephropathy
1, pay attention to rest: patients with kidney disease, during the acute attack should be appropriate bed rest, severe symptoms should be absolute bed rest. Chronic patients should combine work and rest, eliminate worries, maintain physical and mental happiness, and avoid labor and strain. If the condition is quite stable and improving, you can participate in some work within your ability.
2, mental health: the patient's thinking, living and working conditions, the necessary health knowledge and knowledge about diabetes, eliminate the fear of the disease and pessimism, and enhance confidence in overcoming the disease.
3, dietary guidance: diet is extremely important, control carbohydrate intake, in order to reduce the burden of pancreatic islet β-cells. Eat more nutritious food containing many kinds of vitamins and proteins. Such as: lean meat, eggs, beans and vegetables, etc., three meals according to the calories in the morning, afternoon and evening each 1/5, 2/5, 2/5 distribution. Make the patients and their families understand the importance of diet to the disease, so that the patients consciously control their diet.
4. Monitoring blood glucose changes and correct injection of insulin: teach patients and their families the correct way to monitor blood glucose and the normal value of blood glucose, so that patients and their families know the injection method, site, time and precautions, such as blood glucose fluctuations should be immediately outpatient review, and do not adjust the dose of insulin by themselves. If there are palpitations, hunger, cold sweat, etc., which are symptoms of hypoglycemic reaction, patients should eat or drink sugar water immediately.
5、 Glucose-lowering drugs: take glucose-lowering drugs at regular intervals according to the doctor's instructions, and pay attention to the observation of the efficacy and adverse reactions, commonly used sulfonylureas such as euglycemic, biguanides such as hypoglycemic and α-glycosaminidase inhibitors, such as Baisuprine, the former two should be taken 30min before meals, during the period of use of the drug, if there is a rash or gastrointestinal symptoms such as nausea, vomiting, etc. should be promptly to the hospital; the latter should be taken at the same time as the first meal to prevent the occurrence of postprandial hyperglycemia. The latter should be taken at the same time with the first meal, mainly to prevent the occurrence of postprandial hyperglycemia.
6, prevention of infection: due to poor resistance of diabetic patients, easily infected, should go to fewer public places, climate change should be timely increase or decrease the clothes, such as colds should be treated in a timely manner.
7. Pay attention to personal hygiene: diabetic patients are prone to boils and carbuncles, etc. They should keep their skin clean all over the body, take baths, change underwear and linen frequently, and keep bed sheets clean. If skin infection occurs, it should be treated in time, and keep the mouth clean, brush the teeth in the morning and evening to avoid oral diseases. 8. Regularly check your blood glucose in the hospital, report your condition and medication to the doctor, and keep track of the dynamic information on the change of your condition.
Recently, several patients with diabetic nephropathy or renal failure have been admitted to the ward, with varying degrees of severity and length of history. Some of them have developed very serious symptoms of uremia, with repeated nausea and vomiting, heart failure, and poor quality of life, and all of them are relatively ill, and some of them have started dialysis treatment.
Diabetes as a silent killer, the name is not for nothing, it is in the silent invasion of your body organs, leading to a variety of early damage, as hypertonic urine excretion of the kidneys, all the time by the impact of sugar, the damage when the brunt.
Renal damage in diabetics usually occurs in the context of chronic poor glycemic control. Chronic hyperglycemia causes renal injury through the formation of advanced glycosylation end products, activation of protein kinases, and acceleration of the aldose reductase pathway. Diabetes mellitus has now become the leading cause of end-stage renal disease, accounting for 20-43.8% of all kidney diseases.
What are the symptoms of diabetes when kidney damage occurs?
When looking at the course of the disease, some people say, "I don't feel sick, right? My blood sugar control is not good, but I'm on medication every day!
Aren't kidney lesions swollen? How did you get to a UTI all of a sudden when you just noticed the swollen eyes?
I look for bubbles every day when I pee, and I don't find any, do I? There's a problem with the kidneys!
This is a concern for many people with diabetes combined with kidney disease.

Patients with kidney damage may have non-specific symptoms such as swollen eyelids, acidity, weakness, back pain, nausea, vomiting, etc. When diabetics experience these these symptoms, the kidneys have been more obviously damaged.
Early symptoms of diabetic nephropathy are very inconspicuous or even without any symptoms. When the patient develops the above symptoms, serious damage to kidney function may have already occurred and the condition has reached an irreversible level, which is very unfortunate.
Therefore, it is very unreliable for many people to stare at their urine and judge whether their kidneys are in trouble based on the presence or absence and amount of foam.
How can we know we have kidney damage when the symptoms are not very reliable?
Patients with type 2 diabetes mellitus are often unable to determine the time of onset of the disease and lack information on long-term follow-up. Currently, the urinary albumin excretion rate is usually used as an important reference index for the diagnosis and staging of diabetic nephropathy.
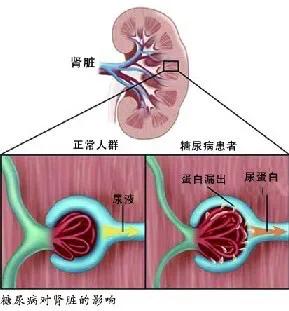
Urine microalbumin
The plasma in the glomerular capillaries enters the renal capsule through the filtration membrane, which is composed of capillary endothelial cells, basement membrane, and peduncles of the foot cells of the dirty layer of the renal capsule. The capillary endothelial cells have many small holes with a diameter of 70-90 mm, called window pores, and the window pore structure only allows small molecule solutes and small molecular weight proteins to pass freely, which constitutes a molecular barrier. In addition, the surface of endothelial cells is rich in negatively charged glycoproteins, which constitute a charge barrier that prevents the passage of negatively charged proteins.

Under normal conditions, medium molecular weight negatively charged albumin cannot be filtered by the glomerulus due to the presence of molecular and charge barriers. Glomerular proteinuria occurs when the glomerular capillary wall barrier is damaged and the cytoskeletal structure of the podocytes and the slit membrane or basement membrane are impaired, and a large amount of protein in the plasma is filtered and exceeds the glomerular reabsorption capacity.
Microalbuminuria is an early clinical manifestation of diabetic nephropathy and is currently the main basis for the diagnosis of diabetic nephropathy.
There are many factors that influence urinary albumin excretion, lack specificity, and are relatively unreliable. The diagnosis needs to be made by reviewing the results in 3-6 months, exceeding the threshold value in at least two out of three results, and eliminating the influencing factors.

Influencing factors include strenuous exercise within 24 hours, infection, fever, congestive heart failure, significantly elevated or fluctuating blood glucose, pregnancy, significantly elevated or violently fluctuating blood pressure, urinary tract infections, prostatitis, or prostate obstruction, all of which can be very misdiagnosed as positive for urine microalbumin or urine protein. When it is not yet possible to test the urine protein/creatinine ratio, patients are usually asked to perform urine tests for 3 consecutive days to rule out influencing factors.
Urine protein/creatinine ratio
The value of the urine protein/creatinine ratio (ACR) is more stable in comparison, and the test is more convenient, requiring only a single random morning urine test, and has now replaced the urine microalbumin test.
diabetic retinopathy
Another basis for early detection of kidney damage is diabetic retinopathy.
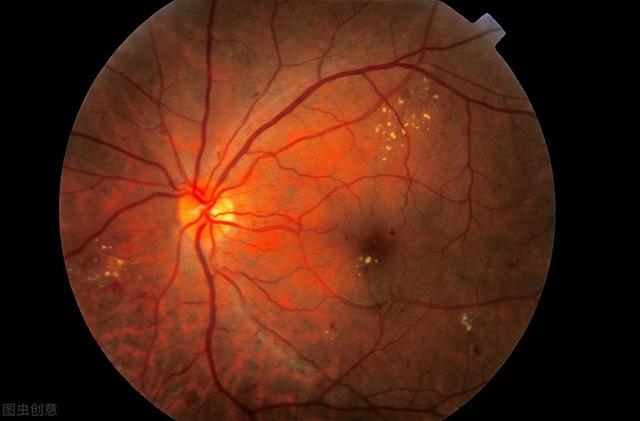
Diabetic retinopathy is also caused by diabetic microangiopathy, and most patients with diabetic nephropathy also have diabetic retinopathy. Therefore, diabetic retinopathy is used by the guidelines as one of the diagnostic bases for diabetic nephropathy in patients with type 2 diabetes mellitus.
glomerular filtration rate
Altered renal function is an important manifestation of diabetic nephropathy. The main indicator of renal function is glomerular filtration rate. Staging of chronic kidney disease can be done based on glomerular filtration rate and other evidence of renal injury. According to the findings, some diabetic patients have no urinary albumin, but the glomerular filtration rate has also decreased. Therefore glomerular filtration rate can be used as one of the diagnostic basis for diabetic nephropathy.
The 2014 Chinese Consensus recommends the modified MDRD formula developed by the Chinese Collaborative Group on Predicted Glomerular Filtration Rate in 2006, which is applicable to the Chinese population, for calculating the glomerular filtration rate to evaluate the degree of renal injury.
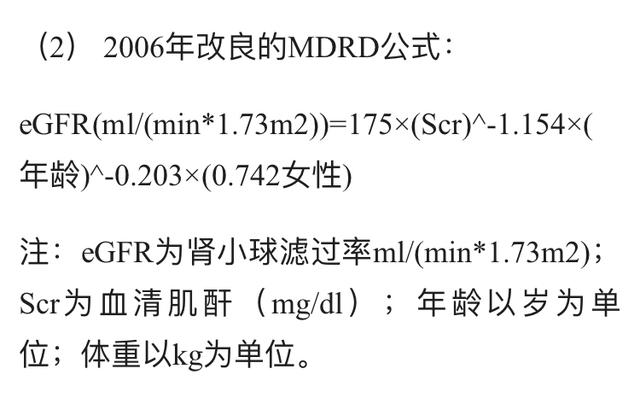
However, in this formula, blood creatinine is not sensitive enough and is easily interfered by individual muscle mass, protein intake, metabolic levels in the body, hemolysis, and other factors. Cystatin C is now considered to be better than blood creatinine in predicting the progression of type 2 diabetic nephropathy to end-stage renal disease.
However, because of the importance of glomerular filtration rate and urinary albumin, both of these tests remain current screening tests for diabetic nephropathy and should be performed annually once diabetes is diagnosed.
Screening programs and requirements
All patients with type 2 diabetes mellitus should be evaluated for urinary microalbumin and urinary protein from the time of diagnosis, and in patients with type 1 diabetes mellitus with a duration of more than 5 years, once a year.
All adults with diabetes mellitus, regardless of urinary microalbumin and urinary protein, should have their serum creatinine checked at least once a year and use it to estimate the glomerular filtration rate, which needs to be staged if nephropathy is present.
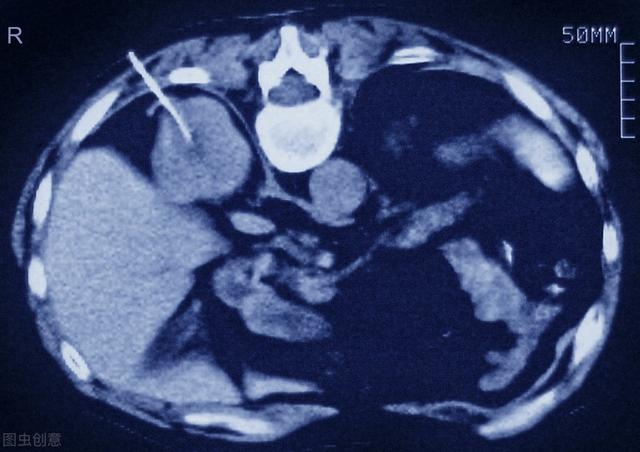
CT scan of a kidney biopsy
Renal biopsy for pathologic clarification
In addition to biomarkers derived from blood and urine, renal biopsy may be an effective way to predict regression of diabetic nephropathy. However, renal biopsy is an invasive test that is very inconvenient in clinical practice.
To summarize:
The diagnosis of diabetic nephropathy is still being explored, and self-perceived symptoms are very unreliable. After diagnosis of diabetes mellitus, regular renal examinations are performed. According to the current consensus, we should not only focus on urinary albumin, but also calculate the glomerular filtration rate, in order to prevent the missed diagnosis of urinary protein-negative diabetic nephropathy, and recommend patients to undergo renal puncture biopsy if necessary, to obtain a clear pathological diagnosis, and to carry out timely and accurate treatment.
The complications of diabetes are particularly numerous, with the most common being diabetic microangiopathy, including diabetic nephropathy, diabetic fundopathy, diabetic foot, and diabetic peripheral neuropathy.
Diabetic nephropathy is a common and troublesome complication. Diabetic nephropathy can cause renal failure and eventually lead to uremia.
The main symptoms of poor kidney function in diabetic patients are the following
1. Swelling: the face, especially the eyelids, are swollen in the morning, and the lower limbs are swollen in the afternoon. The main reason is that after kidney injury, protein leakage from the urine leads to hypoproteinemia.
2. Urine abnormalities: there can be a decrease in the amount of urine compared with the previous, the urine contains more foam. Laboratory tests can see proteinuria and urine sugar positive.
3. Anemia: In the late stage, renal anemia may appear, manifested by weakness, memory loss, cold fear, etc..
4. Hypertension: Some patients may experience increased blood pressure.
5. Itchy skin: In the late stage, some patients develop itchy skin, mainly due to uremic toxins.
Glad to answer this question. Diabetic nephropathy is one of the important complications in diabetic patients. The incidence in our country is also gradually on the rise, so it is important to correctly recognize the symptoms in diabetic patients with poor kidney function.
Here we will learn more about the symptoms of diabetic nephropathy.
1. Proteinuria.Intermittent proteinuria is the first clinical manifestation in patients with diabetic nephropathy, after which it will develop into persistent proteinuria. If the diabetes is well controlled, proteinuria may persist for many years without abnormal renal function. If it is not well controlled, azotemia and renal insufficiency will develop.
2. Edema.Patients with advanced diabetic nephropathy will show signs of edema due to large amounts of proteinuria.
3. Hypertension.Symptoms of hypertension appear relatively late. Alterations in the structure and function of the renal resistance vessels and sodium retention in diabetic patients are the main reasons for the development of hypertension.
4. Mild to moderate anemia.Patients with diabetic nephropathy who have significant azotemia may have mild to moderate anemia.
5. Retinopathy.Diabetic-onset nephropathy is often associated with retinopathy.
Move your fingers and click like! Welcome to SugarManHealth.com!
Diabetic complications are a serious threat to the human body. Involvement of large blood vessels can cause diabetic heart disease, diabetic cerebrovascular disease, diabetic foot; Involvement of microvessels can cause diabetic retinopathy, diabetic nephropathy; Diabetic nephropathy is one of the most typical microvascular complications, and once it develops to the end stage, it will threaten the human body's health, and even life, so the early prevention and treatment of diabetic nephropathy is particularly important.
Diabetic nephropathy is insidious and not easy to be detected. At the initial stage, there may be no clinical symptoms, and the renal function examination may be in a normal state, and only when the disease develops into clinical diabetic nephropathy will it manifest as proteinuria, and then a series of abnormal manifestations such as edema and high blood pressure may gradually appear, and the degree of abnormality of these manifestations often reflects the degree of damage to the renal function.

Clinically, diabetic nephropathy is divided into five stages according to the degree of renal function impairment.Stages I and II have no obvious clinical symptoms except for changes in laboratory renal function and changes in renal volume, and the impairment of renal function can often be reversed with insulin therapy.Stage III is early diabetic nephropathy, which occurs when blood glucose is not well-controlled for a long period of time, and occurs after 15 years of the disease.During this period, there is a blood pressure Elevation.
Stage IV for diabetic nephropathy, the disease develops to this stage, some patients appear a large amount of proteinuria, edema, hypertension performance.V stage for end-stage renal failure, is also the most serious period of the disease, the development of this period, often accompanied by diabetes other microvascular complications. In short, diabetic patients in addition to testing blood glucose if diabetic patients continue to foamy urine, edema and other manifestations, it is necessary to carry out further examination of renal function in a timely manner.

Answer: Gao Xiaoqian, M.S., M.A.
Welcome to Life Calling for more useful health knowledge.
Diabetic nephropathy is now a high incidence of a kidney disease, this disease is very harmful to the human body, most patients with diabetic nephropathy will appear proteinuria, hypertension, edema, nephrotic syndrome and renal failure, and in severe cases will even jeopardize the life of patients with diabetic nephropathy, diabetic nephropathy, patients with what are the obvious symptoms? Many people do not understand this very well, the following is a specific introduction to this issue.
Proteinuria: This is the first sign of diabetic nephropathy and the only manifestation in the early stage. During the period, proteinuria is intermittent and gradually develops into persistent, and urine microscopy can find leukocytes and tubular pattern. When persistent proteinuria occurs, the glomerular filtration rate begins to decline. As the disease progresses, the amount of urinary protein gradually increases, and the amount of urinary protein is consistent with the severity of renal lesions. When the glomerular filtration rate is significantly lower than normal, after the emergence of a large amount of proteinuria, can quickly develop into renal failure. If the 24-hour urine protein is less than 3 grams, there is no significant increase in the amount of urine protein, the progress of renal failure becomes slow.
Edema and nephrotic syndrome: about half of diabetic nephropathy patients present with edema, which may be due to hypoproteinemia caused by the loss of large amounts of protein in the urine, but the older the patient, the more causes of edema caused by other reasons, and about 20% of diabetic nephropathy patients will have nephrotic syndrome.
Hypertension: this is a more advanced diabetic nephropathy symptom, appearing in diabetic nephropathy patients who have proteinuria for a longer time. Initially, the blood pressure increases only after exercise, and when there is persistent proteinuria, the blood pressure increases more continuously, and the appearance of hypertension accelerates the deterioration of renal function in diabetic nephropathy patients.
Renal failure: in the early stage to adapt to the needs of sugar excretion, glomerular filtration rate increases, blood urea nitrogen and creatinine levels are normal, after the emergence of persistent proteinuria, blood urea nitrogen and creatinine concentration increases, the manifestation of renal insufficiency, diabetic nephropathy patients within a few years can be developed to end-stage renal failure. In addition, diabetic nephropathy is often accompanied by a variety of complications, heart failure and cystitis and other complications often affect renal function, ketoacidosis and hyperosmolar coma with circulatory failure, acute renal failure can also occur.
The above is the diabetic nephropathy patients will have what obvious symptoms of the specific content, I believe that you have already understood, only fully understand the knowledge of diabetic nephropathy, diabetic nephropathy patients can be better to accept the treatment, and its therapeutic effect can be better.
With the popularization of science in recent years, many people are not unfamiliar with the dangers of diabetes. Everyone already knows that the most dangerous thing about diabetes is the complications. And the kidneys are the focus of diabetes attack, especially need to pay attention to.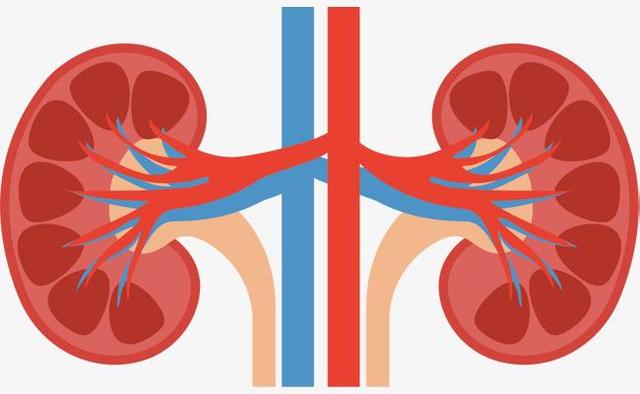
Kidney damage caused by diabetes is called "diabetic nephropathy". It is staged, from early (stage 1) to late (stage 5), stage 5 is the uremia stage, which requires dialysis to maintain life, not to mention the cost and suffering, the quality of life is extremely low. Therefore, it is very important to detect kidney function abnormality at an early stage.
We generally rely on three things to find out the disease, one of which is clinical symptoms, which are all kinds of discomfort in the body, such as dizziness, chest pain and so on. The symptoms of diabetic nephropathy are as follows: increased nocturia, getting up four or five times a night; fatigue, feeling spiritless and weak; in addition, there are dizziness, decreased sexual function, etc., but it is not specific, and the main thing is that there is more nocturia and fatigue.

The second is physical signs. That is, the body is different from normal. The main sign of diabetic nephropathy is edema, which is common on the back of both feet, calves and other parts of the body. Another important sign is high blood pressure. When a diabetic patient's blood pressure used to be normal, but recently increased to be alert to whether the kidney problem.

The third is auxiliary examination. Including a variety of blood tests, urinalysis, ultrasound, CT and so on. Important auxiliary tests for diagnosing diabetic nephropathy include: positive urine protein, elevated blood creatinine and so on. When diabetic kidney damage is suspected, the doctors in the hospital will check for you in detail, so you don't need to worry. Just remember when you find positive urine protein and elevated creatinine, it is kidney damage.
If diabetic nephropathy is found and diagnosed only by these conditions, most of them are stage 3 or above, and the treatment is not very effective. It is better to find out before stage 3, then the healing will be quite good. But can it be detected? Yes! But not by signs and symptoms, but by a simple test: urine microalbumin. Note that it is not a routine urine test, which does not allow early detection, it must be a urine microalbumin. It is recommended that diabetics check every six months to avoid a lot of trouble later in life.
"The best way to prevent diabetic nephropathy is to save for a rainy day. Of course, if you miss stage 1 or 2, you can still remedy the disease if you find it in stage 3, "it's not too late to mend". Don't delay until stage 4 or 5 to think about the treatment.
The typical symptoms of diabetes are three more and one less, but each patient is different and not everyone will have symptoms, and may only have some typical symptoms when they are severe.
When diabetic kidney function is in question, in the early stages of diabetic nephropathy, there are likely to be no clinical symptoms, which manifests itself only as microalbuminuria.
If at this time the patients do not pay attention to their indicators in this regard, or do not go to the hospital regularly to do quantitative urine microalbumin or urine ACR examination, and do not notice the abnormalities, then it is very difficult to find out that they have diabetic nephropathy.
However, the manifestation of abnormal kidney function may be different for different types of diabetes, such as type 2 diabetes, which has basically no typical symptoms as mentioned above. It is basically difficult to find out that there is a problem with the kidneys if you don't go for a checkup.
However, patients with type 1 diabetes may experience the typical three highs and one low, which are manifested in excessive drinking, eating, and urinating, weight loss, and the person becoming thin, among other things.
When diabetic nephropathy develops further, stage II and III, edema, foamy urine, back pain and fatigue may occur.
Further progression of the disease, a large amount of proteinuria causes hypoproteinemia, which will be manifested as edema and decreased renal function.
In advanced renal failure, anemia, malaise, nausea, vomiting, decreased urine output, and poor natriuresis, as well as clinical manifestations such as abdominal effusion and pleural effusion.
Therefore, the general symptoms of diabetic nephropathy are different at different stages, and the early manifestations of type 1 and type 2 diabetes are not the same.

How do you combat diabetic nephropathy?
Diabetic nephropathy can be prevented and treated as follows:
1、Blood glucose control: monitor blood glucose regularly, control blood glucose within a reasonable range, after the occurrence of diabetic nephropathy, you can use hypoglycemic drugs or insulin therapy, adhere to a low-sugar, low-fat, low-salt diet, high-quality protein diet, appropriate exercise, regular work and rest, quit smoking and drinking;
2、Control blood pressure: make the blood pressure stabilize in the normal range, for diabetic nephropathy can use ACEI or ARB class drug treatment;
3、Regular monitoring: regular testing of 24-hour urine protein, urine microalbumin, β-microglobulin, patients with diabetic nephropathy should strictly control protein diet;
4、Control edema: diabetic nephropathy patients can relieve severe edema symptoms by diuretics.
In general, the clinical manifestation of diabetic nephropathy is the symptoms of diabetes mellitus plus the symptomatic manifestation of nephrotic syndrome, which is basically the symptoms of diabetes mellitus such as three more and one less plus foamy urine, swelling, and early urination which are the changes of nephropathy.
Because diabetic nephropathy is likely to have no symptoms in the early stage, keeping an eye on your body's indicators and having regular medical checkups is a good way to prevent and treat diabetic nephropathy and other complications.
Diabetic nephropathy is one of the microvascular complications caused by long-term hyperglycemia in diabetic patients, and is an important cause of chronic kidney disease and end-stage renal disease (kidney failure).
Clinical symptoms include proteinuria, hypertension, edema, etc. Renal function tests often indicate abnormal renal function, decreased urinary albumin and glomerular filtration rate. Some patients may have anemia, and often combined with other microvascular complications, such as diabetic retinopathy, diabetic peripheral neuropathy and so on.

Once you have diabetic nephropathy, you should be prepared to fight a long-lasting war, not only need to actively control blood glucose, diet also needs to be a high-quality animal protein diet, avoid excessive intake of high vegetable protein foods such as soy products, and should not eat too much high-fat, high-calorie foods, the choice of medication should be active to reduce urinary protein, improve kidney function.
1. There will be intermittent proteinuria, which will later develop into persistent proteinuria
2. Edema, diabetic nephropathy due to a large amount of proteinuria will appear edema performance
3. Hypertension, the symptoms of which appear relatively late in life
4. anemia, diabetics with significant azotemia will have mild or moderate anemia
5. Retinopathy: the appearance of diabetic nephropathy is often accompanied by retinopathy

This question and answer are from the site users, does not represent the position of the site, such as infringement, please contact the administrator to delete.