What are the key points of insulin injection?
Some diabetic friends need insulin treatment, in the hospital doctors and nurses speak clearly, but when they use, or some nervous, feel very unsure, so use in the end is not right? What should I do if I make a mistake in injection?
Here to remind all the insulin use diabetic friends and family, when the first time to use insulin, usually in the hospital to use, be sure to understand the main points in the use of insulin, it is best to be able to operate under the guidance of the nurses, the use of the process of the uncertainty of the place to ask a few times, to prevent the "eyes to understand, but the hand did not keep up! "The best thing to do is to ask the nurse several times about what you don't know in the process of using insulin.
It is best to have a family member or a child accompanying you so that you can remind each other of areas you are unsure of when injecting insulin at home .
Premixed insulin and intermediate-acting insulin should always be mixed when used
Some people with diabetes may not be quite sure what type of insulin they are using, exactly, they can't say, but clear, muddy water is what many people like to say.
To teach you an easy way, take an insulin and if you find it is cloudy, then it is something that needs to be shaken well before you can use it.
This is a very important step in the insulin injection process, and if it is not shaken, then the concentration of the two pre-mixed drugs is not the same at the beginning and the end of an insulin administration, leading to fluctuations in blood sugar.
Selection of insulin injection sites
The most suitable part of the body for insulin injections
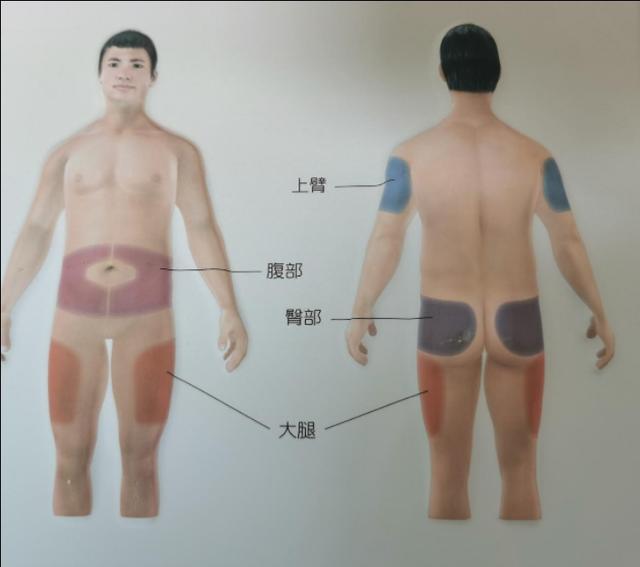
The most suitable areas of the body for insulin injections are the abdomen, the front and outside of the thighs, the outer and upper buttocks and the outside of the upper arms. These skins should not have scars, wounds, infections, tattoos, etc.
Priority is given to the abdomen. The appropriate site for the abdomen is all parts of the abdomen outside the 2 transverse fingers around the umbilicus; this site has the most stable insulin absorption and is less painful, with relative skin delivery and a wider selection area that facilitates single patient manipulation.

Lateral thighs and anterior thighs, to avoid the inner thighs, usually need to pinch the skin, this part of the skin is tighter, and the distance between the muscle is relatively close, easy to inject into the muscle layer and speed up the absorption of the drug.
Hip injection is more inconvenient, but also an injection site for insulin, because the subcutaneous tissue in this area is thicker, it is not easy to inject into the muscle layer, but it is inconvenient for a single person to operate, and generally injected by other people can choose this site.
The least suitable area for self-injection is the upper arms, where the fat layer is relatively thin and the skin needs to be pinched up for safe injection.
Insulin injection sites need to be rotated frequently
Insulin injection sites need to be rotated often, and if you don't, it's time for that skin to give its opinion! (What am I doing wrong?) Rotation of injection sites can avoid the trauma caused by repeated injections in the same area, reduce localized fat growth and atrophy, and prevent poor absorption of medication that may not achieve the desired effect.
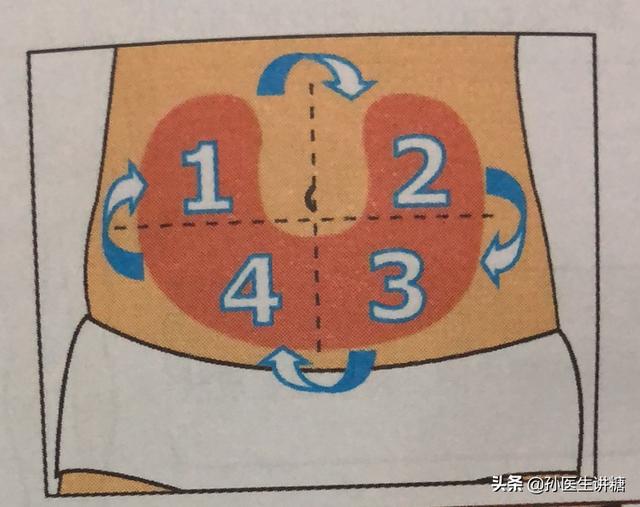
For the rotation method, in the case of the abdomen, for example, the injection site can be divided into 4 quadrants, and injections can be performed weekly in one of the quadrants, rotating in a clockwise or counterclockwise direction.
When injecting in any part of the body, the distance from the last injection point is 1 cm or more to prevent pain caused by heavy injections.
Angle and needle selection for insulin injection
The angle of insulin injection should be determined according to the body shape of your diabetic friend
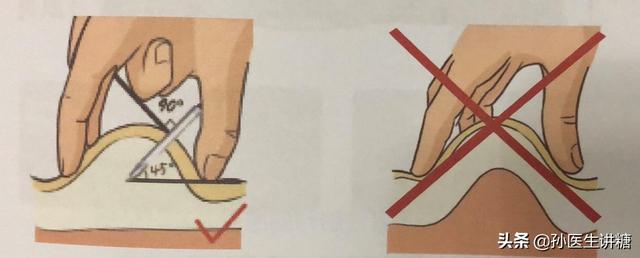
In children and thin adults, the needle is inserted at a 45° angle, and the skin is pinched up before injection to ensure that the insulin is injected effectively and accurately under the skin. The skin is pinched with the thumb, index and middle fingers so that the fat layer is pinched up. It is very easy to pinch the muscle layer with more than one finger.
Vertical needle entry is sufficient for normal weight and overweight adults.
Insulin injection needles
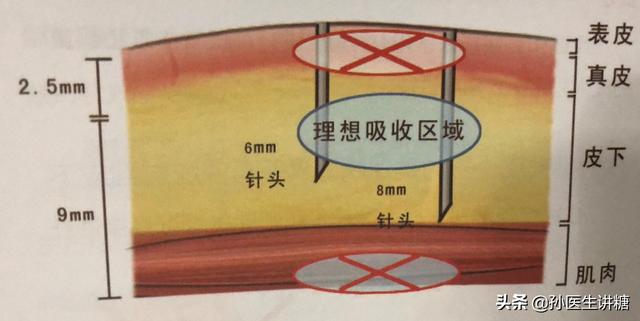
Currently used needles are 6-8 mm, the needle is not easy to bend and destroy, multiple reuse of diabetic friends can choose, but 4-6 mm needle injection is safer, the thinner the needle, the lower the chance of pain and bleeding.
Although the needle we are repeatedly emphasized that repeated use is strictly prohibited, because the repeated use of needles will cause deformation of the tip, and may even break in the body, while the naked eye is difficult to detect these changes, it will increase the pain and fear of injection. However, as can be seen from the survey, many diabetic friends are still reusing them, and it is recommended to minimize the number of times they are used, and to cover the needle cap and pen cap after use to prevent contamination.
Precautions before and after injection
Pre-injection:
1. Check the amount of drugs in the pen, whether it is enough for this injection, to replace the new refill in a timely manner, to prevent the possibility of injecting into the second injection only to find that the amount is insufficient, to avoid not wanting to inject again and lead to insufficient dosage of the situation, it is necessary to look at the amount of drugs beforehand to see whether it is enough.
2. Sterilize with alcohol and inject after the alcohol dries to prevent the alcohol from irritating the needle eye and causing pain.

3. Ventilate before injection, rotate the dosage to 1u, with the needle tip upward, push the button and observe whether there is liquid coming out of the needle tip, if so, adjust your own injection dosage for injection, if not, repeat the above action to know that there is liquid coming out of the needle tip. This is an action that must be repeated for each injection to prevent insufficient injection of medication that may lead to unsatisfactory blood glucose control.
Post-injection:

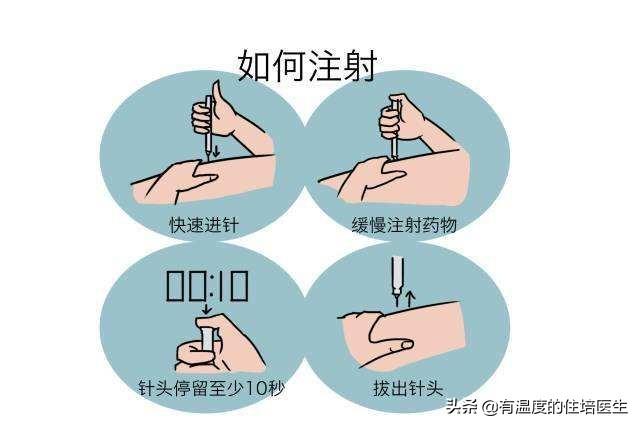
1. After the insulin injection, the pen will make a "snap" sound of locking the button, which means that the drug has been completely injected into the subcutaneous, at this time must not directly pull out the injection pen, to stay for a while, to prevent the needle out of too fast, the liquid will flow out of the skin with the needle. General stay time is 10 seconds, you can count to determine the time such as silent count 1, 2, 3 ...... 10 and so on roughly.
2. After pulling out the needle, use a clean and dry cotton swab to gently press the injection site, do not rub, press for 1-2 seconds.
To summarize: insulin injection is one of the operational skills that diabetics need to master, the injection method is very simple, shaking - volume - injection, only three steps, but there are really very many things to pay attention to, to be constantly adjusted in practice, to ensure that the correct, standardized operation, in order to use the weapon of insulin, will be a good blood glucose control smooth.
I'm Dr. Sun, pay attention to Dr. Sun talk about sugar, continue to learn more quality health knowledge, help please like, have questions please leave a message, will reply!
Here nurse practitioner Yang focuses on one thing: what you need to pay attention to when injecting insulin at home!
Many people with diabetes need long-term insulin injections to stabilize their blood sugar. With the increase in the number of diabetic patients injecting insulin at home, it is not uncommon for patients to "knock themselves out".
So what should you look for when injecting insulin at home?

The main points are as follows:
1. Insulin pens should not be kept in the refrigerator
Clinically, we have encountered many patients who keep both insulin and injection pens in the refrigerator. In fact, it is not advocated to put the insulin already used in the insulin pens in the refrigerator, because it will have some effects on the insulin pens. Therefore, the insulin pen and the insulin inside should be kept outside the refrigerator. At room temperature of 25℃, the insulin can also be kept for 4~6 weeks, while the insulin in the pen will be used up quickly, and there is no need to worry about the deterioration of the insulin in the insulin pen.
2. Selection of injection site
Different injection sites absorb insulin at different rates, so the time it takes for the drug to take effect will vary. The speed of absorption, from fastest to slowest, is as follows: abdomen, upper and outer arms, front and outer thighs, and buttocks. In addition, since repeated injections at the same site may produce hard knots, the injection site and area should be rotated regularly.

3. Handle hypoglycemia in a timely manner
When injecting insulin, hypoglycemia may occur if the injection dose is inaccurate or if meals are not timed and dosed and the injection site is wrong, etc. Hypoglycemia can be life-threatening in severe cases. Therefore, patients treated with insulin must know how to deal with hypoglycemia when it occurs.
Hypoglycemia occurs mainly due to too large a dose of insulin or hypoglycemic medication, taking medication too early or eating too late, forgetting to eat or not eating enough, and being active without adding a meal or adjusting the dose of medication in time. When hypoglycemia occurs, there will be weakness, hunger, dizziness, drowsiness, rapid heartbeat, blurred vision, confusion, etc. At this time, you should immediately eat some high-sugar diets, such as sugar water, cookies and so on. Those who do not get better after the above treatment should go to the hospital for examination quickly.
1、Injection in different parts
The sites of choice can be the abdomen, back of the upper arms, thighs and buttocks, do not inject around the belly button, as shown in the picture below. If you always inject in one area, the skin will react to the penetration of the needle and form red, swollen and hard nodules, affecting insulin absorption. If you need to inject in the same area of the body, the new injection point should be at least one finger's width away from the previous injection point.
2. Use new needles
The needles are specially designed to be very tiny and finely polished to help penetrate the skin more easily. Repeated use can increase discomfort and, crucially, can lead to bacterial infections.
3, to be injected into the fat tissue
Skin structure from outside to inside are skin, fat, muscle, insulin to be injected in the fat tissue. Too deep into the muscle will be absorbed by the muscle and the action time will be shortened, and too shallow, the absorption will be slow, affecting the action of insulin. Therefore, thin people or children should be injected at 45°, and fat people should be injected at 90°. It is also the reason for choosing the above area, which has a thicker fat layer and is easier to find the correct injection depth.
With the development of society and the increase of living standard, more and more people are suffering from diabetes, which is also called a "rich disease". Blood sugar control requires not only diet and exercise, but also oral medication and subcutaneous insulin injection. Most of the time, insulin is injected by the patient himself. Due to improper handling, many times insulin does not work or does not work completely. Here we need to know what are the main points of insulin injection.
Precautions for subcutaneous insulin injection:
(1) Accurate use of medication: familiarize yourself with the names, dosage forms and action characteristics of various insulins, accurately carry out the doctor's instructions, and inject on time!
(2) Suction order: when mixing long and short-acting or medium and short-acting insulin, short-acting insulin should be suctioned first, then long-acting insulin, and then mixed, and must not be operated repeatedly!
(3) Preservation of insulin: unopened insulin is put in the refrigerator at 4~8℃ for cold storage, the insulin being used can be used for 28 days at room temperature (not more than 28℃) without putting it into the refrigerator, it should avoid excessive cold, heat, direct sunlight, violent shaking, etc., otherwise it can be invalidated due to the coagulation and denaturation of the proteins.
(4) Selection and replacement of injection site: When insulin is injected subcutaneously, choose the parts with loose skin, such as upper arm deltoid muscle, gluteus maximus muscle, anterior thigh, abdomen, etc. The fastest absorption is in the abdomen, followed by the upper arm, thigh and buttocks. The fastest absorption is in the abdomen, followed by the upper arm, thigh and buttocks respectively. The injection site should be changed frequently, long-term injection of the same site may lead to local subcutaneous fat atrophy or hyperplasia, localized hard nodules. If injecting in the same area, the injection site must be more than 1cm away from the previous injection site, choose the site without hard knots, such as hard knots, the use of hot compresses, but to avoid burns. Insulin injection should be strictly aseptic to avoid infection.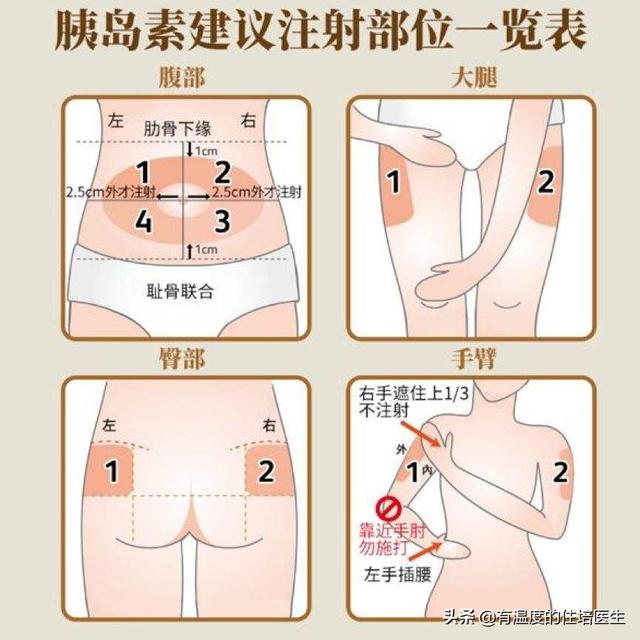
(5) Pay attention to monitoring blood glucose: patients injecting insulin generally routinely monitor blood glucose 2 to 4 times/day, if excessive fluctuations in blood glucose or persistent hyperglycemia are found, the doctor should be notified promptly.
6) When using insulin pens, it is important to pay attention to: the mutual matching of pens and refills, confirming whether there is enough dose in the pen before each injection, and whether the drug solution is deteriorated; in addition, the needles should be replaced before each use, and the needles should be discarded after injection!
Finally, the observation and treatment of insulin adverse reactions: 1, blood hypoglycemic reaction! 2, allergic reaction: manifested as itching at the injection site, followed by urticaria! 3, subcutaneous fat atrophy or hyperplasia at the injection site: the use of multi-point, multi-site hypodermic injections and the timely replacement of needles, which can be prevented from occurring! 4, edema: the initial stage of insulin treatment can be due to water and sodium retention, and mild edema, which can be alleviated on its own!
Summary: Insulin injection needs to be carried out under the guidance of specialized medical personnel, and must not be blindly injected, so as to avoid accidents, causing harm to themselves. We hope that diabetic patients can strictly implement the operation standard, so that insulin can play a real role.
Injection sites for insulin
Insulin is usedhypodermic injectionThe way of injecting into the muscle layer should be avoided. According to the distribution of vascular nerves as well as subcutaneous tissues in the human body, insulin injections are often chosen at the following four sites:Abdomen, middle third of the lateral aspect of the upper arm, upper third of the anterolateral aspect of the thighs bilaterally, and upper lateral aspect of the buttocks bilaterally.。
Insulin is not absorbed at the same rate for different parts of the injection:
Repeatedly injecting insulin at the same site tends to cause subcutaneous fat proliferation and hard knots, leading to decreased insulin absorption, prolonged absorption time, and resulting in blood glucose pulsation, so the injection site should be changed frequently.Patients on long-term insulin use should have regular and planned rotation of injection sites
Insulin Needle Delivery
Currently, the length of insulin needles is categorized into 4 mm, 5 mm, 6 mm, 8 mm, etc., and the appropriate needle should be selected according to body size. Generally speaking, short needles of 4-6 mm are not easy to penetrate into the muscle layer and are safer.
In general: 5mm needles do not require pinching of the skin, 8mm needles require pinching of the skin, and 12mm needles require a 45° feed.
The proper technique for pinching the skin is to pinch up the skin with the thumb and index finger, not with more than one finger so as not to pinch the muscle layer.
Selection of injection sites for different types of insulin
According to the drug release characteristics of different insulins and the absorption rate of different injection sites, a better injection site can be selected for different types of insulin.
Other considerations
1. Before using insulin, you should pay attention to observe whether theCrystallized or flocculent, as soon as it is discovered, it is immediately deactivated.
2. The injection pen should be gently shaken before using premixed insulin to make itmix evenly. This is done by slowly rolling horizontally 10 times, then up and down 10 times, mixing well before use.
3. Before injectionChecking the injection siteWhether there is scarring, hardness, indentation, tenderness and signs of inflammation, and if so, change to another site for injection.
4,75% alcohol should be sterilized before injection.
5. Attention should be paid to the exhaust before injection.Inadequate venting can lead to inaccurate dosing. The correct method of venting is to dial the dose adjustment knob to 2 U , with the needle tip up and upright, flick the quill holder with your finger several times so that the air gathers in the upper part, and then press the injection button until a drop of insulin overflows from the needle, which means that the piston rod has made complete contact with the quill and the air bubbles in the quill have been exhausted.
6. Needle under the skin after the injection of the medicine is completedDwell more than 10 secondsRemove the needle again to ensure that the insulin is fully injected into the body; if the needle is removed too soon, it may cause the insulin to flow out. The dwell time can be extended to more than 15 seconds in the case of larger injected doses.
7. Needles will show obvious changes after repeated use, and repeated use will cause injection pain and the possibility of fracture. In addition, insulin crystals will remain in the used needle, clogging the needle, affecting the effect of use and increasing the risk of infection. Therefore, it is recommended thatUse a new needle for each injection。
Eating fungus can really lower blood sugar? Adhere to 2 points, not half a month, diabetes swept away, no longer rebound!
Can clean eating fungus really lower blood sugar?
Answer: It's impossible~! Although diabetes can eat fungus, traditional Chinese medicine believes that often eat fungus can play a muscle blood, clear the lungs and gas, laxative, remove blood stasis and new, nourishing and strong function, fungus is also a kind of fungal food containing a variety of nutrients, including proteins, fats, a variety of vitamins, sphingolipids, lecithin, lecithin, dietary fiber, mannan, collagen, fermentation, xylose, glucose, Alkaloids and a variety of trace elements, but the role of these, but the real role for blood sugar or a little bit of it, can not achieve the purpose of lowering blood sugar, occasionally eat a little bit is not a bad thing.
Adhere to 2 points, within half a month, diabetes is swept away, no longer rebound!
1. Reduce the rise of blood sugar
The blood sugar of any diabetic almost always rises fast and fluctuates greatly, once the blood sugar rises, it breeds more diseases and also speeds up the arrival of complications, although it is said that there are numerous factors that contribute to the formation of diabetes, but it can never be separated from the point of blood sugar.
Therefore, only the real blood sugar down, diabetes can be cured, the current clinical effect is better "astragalus ketone oil", for diabetes to improve the effect is very significant, and will not rebound, deeply diabetic people's favorite.
However, "Astragalus Ketone Oil" is usually recommended to take more than 3 months, most people will see the effect in about 3 months, the slowest is also 6 months to see the effect.
2. Self-relaxation and emotional regulation
Relaxation exercises such as deep breathing and relaxing muscles with relaxing music can help relieve stress and make glucose therapy more effective. Learning to regulate emotions and enhance self-efficacy to overcome fear and negativity after illness can also help control blood glucose.



For some "sugar lovers", insulin is the "special drug" for diabetes. Choosing the right needle, using the needle correctly, choosing the right angle of needle insertion, and how long the needle is left in place have an important impact on long-term blood glucose control. The following is a detailed explanation by Wu Xianhui, Head Nurse of Internal Medicine Department of Chongqing Sanbo Jiangling Hospital.
Needle feed angle
The 4mm and 5mm needles are suitable for all adult patients (including obese patients) and usually do not require pinching of the skin during injection, which should be given at 90° to the skin surface.
To avoid intramuscular injection in patients using needles ≥8 mm in length, the skin should be pinched or injected at 45°.
Pinch the skin need to pay attention to: pinch the skin should not be too strong, too large easily lead to white skin or pain. Can not use the whole hand to lift and pinch the skin, in order to avoid the muscle and subcutaneous tissue with the pinch up.
Needle retention time
Press the injection button fully when injecting, the needle should remain under the skin for more than ten seconds after the injection, continue to press and hold the push button until the needle is completely withdrawn, this ensures that the correct dose is injected and stops blood or tissue fluids from the body from flowing into the needle or insulin refill. After injection, unscrew the needle and discard it into the special disposal container and put back on the pen cap.

Optimal injection procedure for patients using needles ≥8 mm in length:
Step 1: Pinch up the skin to form a skin fold
Part 2: After entering the needle at an angle of 90° (or 45°) to the surface of the skin fold, slowly inject insulin
Step 3: When the piston is fully pushed to the bottom, the needle stays in the skin for 10s or 15s (insulin pen injection is used)
Step 4: Remove the needle
Step 5: Loosen the leather folds
What else do I need for my injections?
1. Do not reuse disposable injection needles.
Repeated use can cause the tip of the needle to be deformed or even partially broken off inside the body, whereas it is usually difficult to detect changes in the tip with the naked eye.
Repeated use hazards: increased injection pain, increased chance of needle breakage, increased chance of infection, needle obstruction, causes subcutaneous fat tissue growth, increased chance of contamination of medication.
2. Needles do not need to be sterilized
Disinfectant solutions have the potential to affect the effectiveness of insulin, especially since alcohol wipes can damage the silicified layer (containing a synovial agent) on the surface of the needle and increase pain during injection.
3. Needles should be removed after use and discarded according to the specifications for injection equipment.
Dispose of injection pen needles in a special disposal container; if a special disposal container is not available, a hard-shell container with a lid can also be used.
The dangers of not removing the needle after injection:
When the temperature decreases, the volume contraction of the insulin causes air to enter the cartridge, creating air bubbles and affecting the accuracy of the injected dose.
At elevated temperatures, insulin expands in volume and leaks from the cartridge, wasting insulin and altering the concentration of the mixed insulin.
4、Correct storage of insulin
Unopened vials of insulin or insulin refills should be stored at 2℃~8℃, do not freeze, avoid heat or sunlight, and do not shock.
Insulin in use is stored at room temperature (no more than 25°C-30°C) for 4 weeks after opening, but not beyond the shelf life.
There are these main points to injecting insulin:
1, Preservation. Unopened insulin should be protected from sunlight and freezing, and stored at a constant temperature of 4℃-8℃, while avoiding placing insulin in the freezer, and wanting to return insulin to room temperature before injection.
2, the injection site, according to the fast to slow absorption rate, the injection site has the abdomen (5 centimeters around the navel), the arm on the outside, the thighs in front of the outside, buttocks. Remember to rotate the injection point, not always in a point of injection.
3. Injection dosage. The injection dose should be set by the doctor according to the blood glucose level, and the insulin injection dose should be adjusted according to the blood glucose level.
4. Sterilization. Sterilize with alcohol and change needles one at a time in principle.
5. Avoid hypoglycemia. Be sure to pay attention to eat on time after injection, do not do physical activities or work before eating after injection to avoid hypoglycemia.
This question and answer are from the site users, does not represent the position of the site, such as infringement, please contact the administrator to delete.