How can I change my country's free second-line anti-AIDS drugs?
From March 19, 1987, the U.S. FDA approved the first antiretroviral drug zidovudine (AZT), the U.S. Congress to provide $ 30 million to the states for emergency funding for AZT, which is the history of human history in the history of the fight against AIDS a big step out of the history of human beings, experienced lamivudine, DDI and D4T and nevirapine, efavirenz, klipizide to the current doxorubicin, raltegravir, and other Integrase inhibitors, fusion enzyme inhibitors and so on.
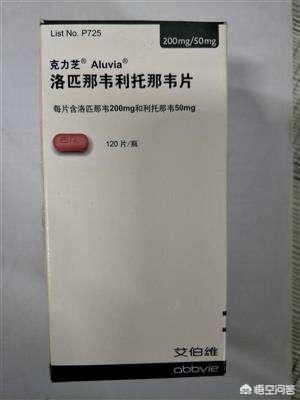
But because the drugs have patents, these drugs are foreign drug companies to develop, and our country does not have a patent, so the beginning of the cocktail therapy are required to import from abroad and then free to the patient, expensive drugs reached several thousand yuan a month, more and more infected people appeared, which also brings pressure to the national prevention and control funds, well after the patent period of the drug our country also began to copy, at present, in addition to the Cliche are At present, except for Cliche is imported, are national generic drugs, and the owner of the question should be the second-line drugs is - Cliche, in our country if you need to replace the second-line drugs need to refer to the current AIDS antiretroviral drug handbook, fourth edition, the content is as follows:
(i) Criteria for inclusion of cases of treatment failure for drug exchange
Patients already receiving first-line therapy must have the following conditions in order to be considered for a new treatment regimen:
1. Patient adherence must first be assessed to determine that the patient has good adherence to the medication and that changing the second-line regimen is not an emergency measure.
2. Patients have received a first-line treatment regimen continuously for at least 12 months.
3. Corresponding standards for the timing of drug changes are now being developed based on the different testing capabilities of each location.
(1) Areas where resistance testing is available: For patients with VL >1000 copies/mL, it is recommended that resistance testing be performed in conjunction with patient adherence assessment and education. When resistance testing shows the presence of a resistance mutation, the drug is changed according to the resistance result.
(2) No access to resistance testing: In areas where viral load testing is available, second-line drug replacement is recommended for patients with VL >5000 copies/mL with confirmation of good adherence.
(3) Failure to obtain timely viral load test results: patients may also be switched to second-line drugs when they experience immunologic failure; the criteria for immunologic failure are as follows (at least one of the following criteria is met):
1) Decrease in CD4+ T-lymphocyte count to or below baseline levels prior to initiation of first-line therapy (2 consecutive episodes separated by more than 3 months).
2) 2 consecutive (more than 3 months apart) decreases in CD4+ T-lymphocyte counts of >50% from peak treatment.
3) For those who have not reached a CD4+ T lymphocyte count of 100 cells/mm3 for more than one year of continuous treatment (it is recommended to confirm adherence to the medication and to be on the lookout for immune reconstitution dysfunction).
4. Given the complexity of the timing of drug replacement, existing clinical staging, CD4+ T lymphocyte counts and VLs are not yet able to fully and accurately assess whether drug resistance has occurred in patients, so drug resistance testing should be sought for patients as much as possible.
(ii) Second-line treatment programs for adults/adolescents
Support for first-line treatment regimens and their adherence must be emphasized, as there is currently a very limited range of antiviral drugs available free of charge in the country. Patients need to understand that the first first-line treatment is the best chance for long-term success on treatment. Support measures for patients include community-based medical staff and professional educators, support organizations, and encouraging family members or closer friends to help patients take their medications as prescribed. Adherence counseling and assessment is performed at each visit. Early detection of non-adherence for a variety of reasons and prompt intervention can significantly reduce virologic failure and the chance of developing drug resistance.
The following steps must be completed before changing to a second-line drug:
(1) Detection of viral load and CD4+ T-lymphocyte count to determine the presence of treatment failure.
(2) Identify whether treatment failure is due to drug resistance or other factors such as adverse reactions or poor compliance.
(3) If drug resistance testing is available, it is recommended that effective drugs be selected based on the test results.
(4) Consult with the Clinical Treatment Expert Group to analyze each patient suspected of treatment failure specifically and document the details.
The Clinical Therapeutic Expert Panel is responsible for selecting the second-line drug for each treatment-failed patient based on medication history, especially previous application of antiviral drugs. If a patient does not recognize virologic treatment failure early on by viral load testing, and treatment failure is judged after several months based on a decline in CD4+ T-lymphocytes or on the development of clinical disease, the patient is likely to have developed resistance to multiple NRTIs. At this point, NNRTIs should not be replaced with just one protease inhibitor, but rather the patient should be selected based on the results of drug sensitivity testing, and the protease inhibitor should be potentiated with an RTV. The boosted PI consists of a small dose of RTV and a larger dose of another PI. the combination of the two proteases has a strong antiviral effect, and when used in combination with two other drugs (two NRTIs), it can even completely suppress HIV again when some degree of resistance has already occurred. the boosted PI instead of NVP or EFV is a new and effective antiviral in patients who have failed treatment. Instead of NVP or EFV, a potentiated PI is a new and effective antiviral combination for treatment-failed patients, and at least one of the other two NRTIs used in combination with a potentiated PI needs to be a completely new drug.
I hope it can help you! About infectious diseases can pay attention to Dr. Li Ping, health road with me!
This question and answer are from the site users, does not represent the position of the site, such as infringement, please contact the administrator to delete.