Can you die from proteinuria?
Hello, I am an attending general practitioner and I hope my answer will help you.
Before answering your question, let's talk about your current state of mind, as you will see from your question, diabetes, tested for urinary proteins, you are very worried about your health condition.
I would like to say that this excessive worry of yours will not only not be beneficial to the treatment of the disease, but will bring many disadvantages.
Studies have found that diabetics who are plagued by depression, nervousness, pessimism, pain and other emotions will gradually aggravate their condition and form a vicious cycle.
Adverse psychological factors can cause a large secretion of some stress hormones in the body, and elevated levels of these hormones can cause diabetes to recur, which is not conducive to the patient's recovery.
Therefore, with diabetes or diabetes complications, are in the best psychological state to take the initiative to accept the treatment, by actively regulating emotions, change the state of mind, and constantly invigorate the spirit, tenacious fight against the disease, to have the confidence and courage to overcome the disease, so as to avoid or mitigate the occurrence and development of acute and chronic complications of diabetes, good state of mind and the correct treatment of the condition, is very favorable to the treatment.
Back to the main topic. Let's talk about diabetic nephropathy.
Diabetic nephropathy is a very common and important complication in diabetic patients. Although the exact cause of diabetic nephropathy is still not clear, it is now generally believed that it is related to poor glycemic control leading to abnormal renal metabolism, and insufficient treatment of diabetic co-morbidities such as hypertension and other diseases.
Diabetic nephropathy can be categorized into 5 stages
Stage 1 is also known as the glomerular hyperfiltration stage, in which there will be no obvious clinical symptoms;
Stage 2, also known as intermittent microalbuminuria, may be associated with hypertension, hyperlipidemia, or metabolic syndrome;
Stage 3, also known as persistent microalbuminuria, is often accompanied by diabetic retinopathy, and if effective treatment is provided in this stage, significant damage to renal function may be avoided;
Stage 4 is also known as the clinical diabetic kidney disease stage or overt proteinuria stage, the patient edema is obvious, the body function is weakened, comorbidities increase, this stage is irreversible, even if the blood glucose control is up to the standard can not prevent it from entering the end stage;
Stage 5 is also known as end-stage renal failure, or uremia, with multiple serious comorbidities requiring dialysis or kidney transplantation.
Therefore, diabetic nephropathy in the early stage of the symptoms are not very obvious, so it is difficult to find, usually in the middle and late stage when the patient will appear a lot of symptoms, such as proteinuria, puffy eyelids, etc., if not treated in time the condition will gradually deteriorate, and there will be swelling of the body, hypo-proteinemia, and other symptoms, and finally lead to diabetic renal failure, uremia and other symptoms of the disease, and the time of survival is gradually decreasing.
First of all, your checkup found urine protein +1, diabetic nephropathy is very likely. But it doesn't completely say that you are diabetic nephropathy, this is also the influence of other factors. For example, caused by urinary tract infection and so on.
From your urine routine urinary protein +1, if diabetic nephropathy, it should also be considered as early stage, and need to measure microurine protein, renal function and other tests again.
So how do you go about discovering diabetic nephropathy?
Aggressive blood sugar control.
By all means. Control blood sugar. For example, strictly limit calorie intake, adhere to the application of hypoglycemic drugs, avoid emotional excitement, infections and other factors that can cause blood sugar fluctuations.
Limit salt intake
In order to protect the kidneys and reduce their workload, salt intake should be less than 6 grams per day, and water intake should be limited in severe renal failure.
When limiting potassium and protein intake
Because diabetic nephropathy is very susceptible to acidosis and hyperkalemia, which will induce cardiac rhythm disorders and hepatic coma, potassium-containing beverages, potassium-containing fruits, and protein intake should be restrained.
Actively treat other underlying diseases. For example, hypertension, hyperlipidemia, coronary heart disease.
When diabetic nephropathy causes hypertension, whether it is type 1 diabetes mellitus or type 2 diabetes mellitus, the preferred pressor drugs are ACEI or ARB antihypertensive drugs, which can control hypertension, reduce proteinuria, and delay the progression of renal function.
It can be treated with herbal medicine.
Back to the initial question. How long can you really live with diabetic nephropathy?
The microalbuminuria that occurs in the early stage of diabetic nephropathy can be improved in some patients after active treatment, while once renal function impairment occurs, it progresses much faster than other glomerular diseases, and diabetic nephropathy develops to end-stage renal failure faster than general kidney disease.
The survival of diabetic nephropathy is closely related to individual factors, disease duration, treatment and intervention, so there is no need to be nervous, active treatment is the first thing to do at present, I wish you an early recovery!
I'm a small doctor of science, and as a medical professional, I'll answer your questions.
Before you can answer this question, you should first know what diabetic nephropathy is.
What is diabetic nephropathy?
According to the 2014 China Diabetic Nephropathy Prevention and Control Guidelines diabetic nephropathy is kidney damage caused by diabetes mellitus, which used to be denoted by DN (diabetic nephropathy), and in 2007 the National Kidney Disease Foundation (NKF) developed the Guidelines for Quality of Survival in Kidney Disease, referred to as the NKF/KDOQI. the guidelines recommend replacing DN with DKD (diabetic kidney disease) instead of DN.
In 2014, the American Diabetes Association (ADA) and the NKF reached a consensus that DKD is defined as chronic kidney disease caused by diabetes mellitus, which consists primarily of a glomerular filtration rate (GFR) less than 60 ml/min/1.73 m2 or a urinary albumin/creatinine ratio (ACR) higher than 30 mg/g persisting for more than 3 months.
Diabetic glomerulopathy (DGN) is specifically defined as glomerulopathy caused by diabetes mellitus as confirmed by renal biopsy.
Diabetic nephropathy has become more and more prevalent in the past few years, and has become the second leading cause of uremia in China after chronic glomerulonephritis.
One necessary point for the diagnosis of diabetic nephropathy is that the duration of diabetes needs to be greater than 10 years, because the vast majority of microangiopathy due to diabetes requires long years of accumulation.
Clinical diagnosis of early diabetic nephropathy relies on 2 main points
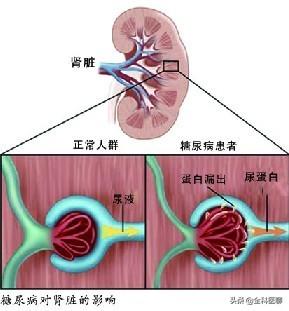
Urinary albumin:Microalbuminuria is an early clinical manifestation of diabetic nephropathy and the main basis for diagnosing diabetic nephropathy.
Diabetic retinopathy:Diabetic retinopathy often occurs earlier than diabetic nephropathy, and the majority of patients with diabetic nephropathy have diabetic retinopathy, but the prevalence of diabetic retinopathy is rather reduced in patients with diabetic nephropathy on dialysis, and diabetic retinopathy is used by the NKF/KDOQI guideline as one of the diagnostic bases for diabetic nephropathy in patients with type 2 diabetes.
Diabetic retinopathy and diabetic nephropathy are both microangiopathies caused by diabetes, and since diabetes is a systemic disease, the two complications are often parallel, meaning that if there is diabetic nephropathy, there will be diabetic retinopathy.
And urine microalbumin is an important means of detecting diabetic nephropathy and is by far the most reliable.
Staging of diabetic nephropathy
Diabetes is divided into 5 stages
Phase I:In the early stage of diabetic nephropathy, glomerular hyperfiltration is the most prominent feature of this stage, with increased renal volume, dilated glomerular arterioles, increased renal plasma flow, increased glomerular intraglomerular pressure, and markedly elevated glomerular filtration rate (GFR).
Phase II:Thickening of glomerular capillary basement membrane (GBM) and mild widening of the mesangial stroma; urinary albumin excretion rate (UAER) is mostly normal, but may be intermittently increased (e.g., after exercise, stress), and GFR is mildly increased.
Phase III:In early diabetic nephropathy, thickening of the GBM and widening of the mesenchymal stroma are evident, and vitrification of the walls of the small arteries is present; persistent microglossia is present.Albuminuria, UAER persisting at 20-200 μg/min (normal <10 μg/min), GFR still above normal or normal.
Phase IV:Clinical diabetic nephropathy, glomerulopathy is more serious, some glomerulosclerosis, focal tubular atrophy and interstitial fibrosis; urine protein gradually increase UAER>200μg/min, equivalent to the total amount of urine protein>0.5g/24h; GFR decline; may be accompanied by edema and hypertension, renal function gradually decline; some patients may be manifested as nephrotic syndrome.
V period:Uremia, most renal units atretic; UAER decreased, blood creatinine increased, blood pressure increased.
And the questioner is currently 1 + proteinuria, the first consideration is diabetic nephropathy stage 3, but still need to improve the 24h urine protein test to see whether it reaches stage 4.
This also tells all diabetic patients the importance of regular medical checkups, as all the complications of diabetes are silent in the early stages, and medical checkups must be needed to detect abnormalities.
Treatment of diabetic nephropathy.
Since you already have diabetic nephropathy, the most important thing is the next step in treatment.
Blood sugar control:Blood sugar control is the most important measure for all diabetic patients. Glucose control is also the only measure that can slow the progression of diabetic nephropathy.Several studies have demonstrated that controlling blood glucose can reduce the occurrence or slow the progression of diabetic nephropathy.Drugs or insulin for blood sugar control, which I do not recommend here, are recommended to go to your local hospital for treatment and strict blood sugar testing. Be sure to follow your doctor's advice, do not change your medical regimen without authorization, and do not stop taking your medication without authorization.
Control of blood lipids:In addition to microangiopathy caused by diabetes mellitus, the causes of diabetic nephropathy include dyslipidemia, atherosclerosis and other chronic kidney diseases, which together cause and promote the occurrence and development of diabetic nephropathy, so controlling blood lipids is also a top priority. Lipid control is mainly to reduce LDL, and the recommended goals of lipid therapy for DKD patients are: LDL-C level less than 1.8 mmol/L in very high-risk patients with a history of atherosclerotic cardiovascular disease or eGFR <60 ml-min-1-1.73 m-2, and less than 2.6 mmol/L in other patients.The main lipid-lowering drug is statin, which can be combined with ezetimibe if necessary.
Control of blood pressure:For patients with diabetic nephropathy, our requirements for blood pressure are relatively strict, requiring blood pressure to be reduced to below 130/80mmHg. If there is no contraindication to antihypertensive drugs, it is generally recommended to use ACEI or ARB class, because these drugs can lower blood pressure at the same time can also reduce urinary protein. The last two words of antihypertensive drugs is Puli is ACEI class, the last word is Tan is generally ARB class antihypertensive drugs.
Smoking cessation:I've typed the word "quit" at least 100 times since entering today's headlines, and I'm not going to recount the dangers of smoking, which can do more harm than good. If you are having a really hard time quitting on your own, we recommend going to a smoking cessation clinic at your local hospital.
Abstinence from alcohol:These two words have been said a million times just like quitting smoking. I've always advocated abstinence rather than limiting alcohol is because I don't trust most self-control. The Lancet is also a call for people to quit drinking, which is harmful in every way.
Movement:This was answered yesterday in response to the topic of controlling blood pressure, but exercise is more recommended for diabetics because it lowers blood sugar.Generally we recommend exercising at least 3 times a week for about half an hour each time for various sports such as jogging, walking, biking and swimming.
Diet:For diabetic nephropathy patients we prescribe a diet that is low in salt, low in fat and high in protein diabetic diet; diet is extremely important for all diabetic patients.It can be summarized as 1234567 mnemonic: 1 egg, 1 bag of milk, 2 taels of lean meat, 3 taels of tofu, 4 taels of fruit, 5 taels of staple food, 6 taels of vegetables, and 7 glasses of water.
If diabetic nephropathy does progress all the way to uremia, then blood dialysis is needed.

summarize
The questioner first of all, do not be anxious first, urine protein 1+ is still relatively early diabetic nephropathy, at this time as long as you do the above points then you can control diabetic nephropathy, so there is no need to be anxious.
So now all you have to do is to do the above from today from this moment to control diabetic nephropathy.
Diabetic nephropathy has also attracted more and more attention, and it is hoped that all diabetic patients will have regular medical checkups to prevent diabetic complications.
Answer:
Diabetic nephropathy, abbreviated as DN, is the result of diabetic microvascular lesions. The clinical manifestation of diabetic nephropathy depends on which stage the patient is in. It initially manifests itself in the form of urinary excretion of microalbumin, then in the form of clinical urinary protein, and finally in the form of chronic renal insufficiency, with end-stage nephropathy being the most important cause of diabetes mellitus-induced death in the elderly.
The first stage is characterized by glomerular hyperfiltration and mild enlargement of the kidneys, i.e., the GFR is already elevated, and also frequently causes a cascade of metabolic dysfunction. The second stage is characterized by rest without increased urinary protein excretion. After exercise, urinary protein excretion also increases and GFR is likely to be higher during this period. It may exceed one hundred and fifty milliliters per minute. Stage 3 is characterized by a persistent increase in urinary protein output, which is the development of early diabetic nephropathy. Stage four, on the other hand, is the clinical nephropathy stage, which is characterized by the development of progressive clinical non-selective proteinuria already, which slowly progresses to glomerulosclerosis. And the fifth stage. Is uremia.
If you are in Stage 1 diabetic nephropathy, here are a few ways to help. Aggressive control of blood glucose levels in the early stages can normalize the growing kidneys as well as normalize the GFR. Secondly, dietary treatment, limiting protein intake in the early stage of diabetic nephropathy can help bring down the high GFR. When consuming protein, use high quality protein and reduce the intake of low quality protein. At the same time, enough calories can be consumed, and vegetable oil can be added when calories are insufficient. The third approach is antihypertensive therapy. The fourth one is ACEI inhibitors. This is the first drug to control hypertension. It not only reduces urinary protein but also reduces glomerular intracapillary pressure. The blood pressure may drop at the beginning of the treatment, so it is advisable to take a small amount at the beginning.
From this question, the subject is very worried and anxious, having diabetes and proteinuria, it is true that you will be very nervous and worried, but if you understand the development of diabetic nephropathy, it may be helpful for the treatment of the disease and alleviate this bad mood.
Diabetic nephropathy is one of the more common chronic microvascular complications of diabetes. It is usually believed that poor long-term glycemic control is the main reason for the development of diabetic nephropathy. However, since diabetic patients are usually combined with hypertension, etc., the possibility of hypertension leading to kidney damage cannot be ruled out.
Proteinuria is present, so which stage of diabetic nephropathy is it?
Let's look at the stages of diabetic nephropathy, which is divided into five stages.
Phase I is the glomerular hyperfiltration phase.
Stage II is a period of intermittent microalbuminuria; patients with stages 1 and 2 have no obvious symptoms and laboratory tests will not reveal significant, persistent abnormalities.
Stage III is the period of persistent proteinuria, which is manifested by the presence of trace amounts of albumin in the urine, usually not exceeding a total of 30 mg/dl per day, and may be accompanied by diabetic retinopathy, which can be reversed to a normal state with effective treatment.
The above 3 stages are called early kidney disease.
Stage IV is also known as the clinical nephropathy stage, where patients develop overt proteinuria in the urine, which manifests as edema, and as the amount of protein increases, renal damage gradually worsens, and impairment of renal function slowly occurs. Generally it cannot be reversed, but good control of blood glucose and blood pressure may slow down the progression of diabetic nephropathy.
Stage V becomes the stage of end-stage renal disease, in this stage there will be renal failure, the state of renal failure, when the body can not compensate, there may be heart failure, severe water electrolyte disorders, the need for dialysis or kidney transplantation and other treatments.
In the case of the subject, because of diabetes, when proteinuria appears in the urine, the first diagnosis that doctors consider is diabetic nephropathy, but urinary protein can also be caused by many factors, such as overly strenuous activities, urinary tract infections and so on. Therefore, we need to observe whether the protein in urine can be excluded from the above factors.
Matters requiring attention:
It is recommended to carry out the examination of morning urine continuously for 3 days, if it is found that all urine proteins are positive, then the diagnosis of clinical nephropathy is established. It is necessary to actively carry out the examination of renal function, electrolytes, renal ultrasound, fundus, etc., to determine your lesion condition and actively treat it.
If you continue to be in the state of proteinuria +, then strict control of blood glucose and blood pressure will slow down the development of renal lesions, clinically, you can see that many patients with positive urinary protein are able to maintain a relatively stable state for many years, which requires adjustments in glucose-lowering and blood pressure-lowering regimens.
In terms of treatment, it is necessary to actively cooperate with the doctor to choose the appropriate treatment program. It is recommended to choose glucose-lowering drugs that do not or rarely go through renal excretion, you can choose such as gliquidone, repaglinide and other urinary stimulants, and it is best to choose insulin for glucose-lowering treatment. Keeping the blood pressure below 135/80mmhg, antihypertensive drugs can choose ACEI and ARB antihypertensive drugs, which have renal protective effects in addition to antihypertensive, and can be considered for use even in diabetic patients with normal blood pressure.
Live on a low-salt, low-fat, high-quality protein diet, with a daily protein amount of 0.8-1.0 mg/kg, less than the amount of protein in non-renal damage diabetic patients, because excessive protein intake may lead to hyperfiltration of the kidneys, resulting in further aggravation of renal damage. Try to choose high quality proteins such as animal proteins and reduce the intake of soy products. The amount of salt should be low, about 3g/day, the amount of a flat spoon in the ingredient box is 1 g. Exercise daily at low to moderate intensity, not strenuously.
To summarize: when diabetic friends find positive protein in urine, they should actively carry out the examination of renal function, electrolytes, renal ultrasound, funduscopy, etc., to determine their lesions and actively treat them. To actively cooperate with the doctor, choose the appropriate lowering sugar, lowering blood pressure and other treatment programs. Take a low-salt, low-fat, high-quality protein diet and exercise in moderation. Don't be nervous, many patients are able to maintain a positive urine protein status for many years without any impairment of kidney function.
I'm Dr. Sun, pay attention to Dr. Sun talk about sugar, continue to learn more quality health knowledge, help please like, have questions please leave a message, will reply!
Diabetic nephropathy or jeopardize the patient's life you know? With the continuous improvement of living standards, the number of diabetic patients is growing at an alarming rate, China currently has nearly 100 million diabetic patients, according to statistics, about one-third of the diabetic patients may have kidney complications.
Poor glycemic control can cause damage to the kidneys, and patients will eventually develop generalized edema, proteinuria, uremia, and die of renal failure. It has been reported that 50 percent of patients with type 1 diabetes have chronic renal failure, while 5 to 10 percent of patients with type 2 diabetes have renal failure. Therefore, the hospital called on diabetic patients to actively prevent the occurrence of diabetic nephropathy.
It is reported that the main clinical manifestations of diabetic nephropathy are: edema, proteinuria, hypertension and renal failure. Specifically, diabetic nephropathy can be simply divided into five phases: Phase I: early stage, the kidney volume increases, no obvious symptoms, urine protein negative; Phase II: glomerular injury period, exercise can appear trace proteinuria, rest can be restored; Phase III, early diabetic nephropathy period, the appearance of microalbuminuria; Phase IV, clinical diabetic nephropathy period, the gradual increase in protein in the urine, which can be accompanied by edema and hypertension, renal function The fourth stage, clinical diabetic nephropathy, urine protein gradually increased, may be accompanied by edema and hypertension, renal function gradually decline; fifth stage, uremia stage.
Nephrologists especially remind: the stage of increased urinary albumin excretion without large amount of albuminuria is called "microalbuminuria", which represents the subclinical stage of early nephropathy, and its appearance not only suggests that the risk of clinical nephropathy is further increased, but also suggests that the risk of macrovascular lesions is increased. Intervention through strict control of blood glucose and blood pressure at this stage is very important to prevent or delay the development of diabetic nephropathy. Therefore, diabetic nephropathy should be prevented in the following ways:
1、Actively controlling high blood sugar is the prerequisite for preventing diabetic nephropathy. Regularly detect changes in blood glucose so that blood glucose is controlled within the target range.
2. Control high blood pressure. High blood pressure will make diabetic nephropathy further deteriorate, should make the blood pressure control at less than 120/80mmHg.
3. Control of high blood lipids.
4, prevention and treatment of urinary tract infections. Frequent urination, urinary urgency, urinary pain timely to the hospital for treatment.
5, try to avoid drugs that have toxic effects on the kidneys, such as gentamicin, streptomycin and so on.
6、Regular physical examination, check urine 24 hours microalbumin, find early kidney disease and early treatment.
Proteinuria does not usually cause death. Proteinuria is a common clinical condition that occurs when there is a urinary tract infection, pyelonephritis, glomerulonephritis, tubular nephritis, or diabetic nephropathy. It is recommended that if you have proteinuria, you should always have further tests to identify the source and decide how to treat it. Proteinuria, it is not serious, so he is unlikely to cause death. Severe proteinuria can cause the body to lose a lot of protein, which may lead to swelling and anemia. If you have proteinuria, pay attention to dietary control, pay attention to light diet, do not consume too much sodium, protein, easy to increase the burden on the kidneys. Normally, you should drink more water appropriately.
If it is just a simple trace of urinary protein, don't be afraid. It usually occurs in normal people after exertion or cold, but it does not last long. If a large amount of proteinuria exceeds 3.5 grams/24 hours, you should seek medical attention. Normally just proteinuria is not life threatening.
This question and answer are from the site users, does not represent the position of the site, such as infringement, please contact the administrator to delete.