Is it reliable for a doctor to say no chemo after bowel cancer surgery?
Should chemotherapy be given after surgery for bowel cancer? It is not something that a certain person decides at will, but it is formulated with reference to the existing medical guidelines, consensus and norms and then combined with the specific situation of the patient. Where do these guidelines, consensus and norms come from? It is the summary of long-term clinical research that most people benefit from the regimen, not all patients.
With the outcome unknown, we can only go with the most likely approach, right?
There are two types of bowel cancer treatment options, one for colon cancer and high rectal cancer according to the colon cancer treatment plan, and the other for low and intermediate rectal cancer to the rectal cancer treatment plan.
Stage I rectal cancer generally does not do adjuvant treatment, while stage II and III are locally progressive tumors, and the standard treatment plan is preoperative radiotherapy, surgery, and postoperative adjuvant chemotherapy according to the situation, while the treatment of stage IV is more individualized, but less chemotherapy.

Chemotherapy is also generally not recommended for Stage I colon cancer, while Stages III and IV are treated with adjuvant chemotherapy, and Stage IV often requires neoadjuvant chemotherapy. The most complex is the postoperative adjuvant chemotherapy regimen for stage II colon cancer.
Stage II colon cancer is divided into stage IIA, IIB and IIC, all of which have no lymph node metastasis and distant metastasis. Stage IIA tumor infiltration depth reaches the subplasma membrane of colon without invading the plasma membrane layer, that is, T3, while stage IIB is the tumor invading the plasma membrane layer T4a , and stage IIC tumor invading the adjacent tissues and organs T4b, and stage IIC is not necessarily able to be operated first.
The decision to have chemotherapy after surgery for stage II bowel cancer is determined by two factors. One is the presence or absence of high risk factors for recurrence (primary focus infiltration depth T4, vascular/neural infiltration, hypo-differentiation, number of lymph nodes detected less than 12, cutting edge too small from the tumor), and it is obvious that IIB and IIC belong to the high-risk factors, while IIA may have no high-risk factors. Another factor is the erratic expression of microsatellites, with a low risk of recurrence with high expression.

Adjuvant chemotherapy is "required" after surgery if there are high risk factors for recurrence.
(ii) Adjuvant chemotherapy is "not required" after surgery if there is high expression of microsatellite instability.
(iii) If there are no high-risk factors for recurrence or high expression of microsatellite instability, then the patient is at generalized risk and chemotherapy is "considered".
"Need", "Don't need", "Consider" are the preferred recommendations, and depending on the patient's physical condition, age, wishes, etc., there are also options for "Observe".
Adjuvant chemotherapy is to reduce recurrence, or prolong the time of recurrence, and close monitoring and rechecking are also required after surgery for early detection and early treatment. Fight cancer scientifically and care for life! I am @Dr. Liu Yongyi , thank you for reading!
With the improvement of living standard, the change of dietary (good fat, low fiber) habit, the change of environment, heredity and other factors, all contribute to the occurrence of intestinal cancer, and the patients may show the change of bowel habit (regular bowel habit becomes constipation or diarrhea, etc.), and some of them are found only when they have lost weight, but the effect of any disease is only good if it is detected and treated early, and the surgical method of intestinal cancer and whether radiotherapy is needed depend on the tumor typing and staging, so you should trust your doctor and relax at the same time. It depends on the type and stage of the tumor, so you should trust your doctor and relax at the same time.
First of all, not all colorectal cancers need chemotherapy after surgery, and a professional doctor needs to make an assessment according to the specific situation.
The need for chemotherapy after colorectal cancer surgery is based on two things.
One is postoperative staging:
This is also the most important criterion to decide whether chemotherapy is given to colorectal cancer after surgery, and the later the staging is, the more meaningful chemotherapy is. For patients with late postoperative staging, because of higher risk of recurrence and metastasis, for these patients, chemotherapy can significantly reduce the chance of recurrence or delay the time of recurrence than no chemotherapy. For example, chemotherapy is routinely recommended for patients with postoperative pathological confirmation of stage III, which is also the standard recommendation for postoperative period; for patients with stage I, generally speaking, active chemotherapy is not recommended.
The second is the risk factor:
so-calledrisk factor, which refers to the patient's additional presence of certain unfavorable factors that increase the patient's risk of recurrence and metastasis in addition to the above staging, such as: preoperative presence of intestinal obstruction or perforation of the tumor site, postoperative pathological results confirming T4 (the tumor infiltrated the intestinal canal), poor histological differentiation of the tumor, presence of a tumor choroidal infiltration, and a tumor neurological infiltration, etc., and the fact that fewer than 12 lymph nodes were sent to be examined, which is also in the risk factor category.
For stage III patients, because of late staging, chemotherapy is required with or without risk factors; for stage II patients, chemotherapy may not be necessary if there are no risk factors mentioned above, while chemotherapy is recommended if there are risk factors mentioned above; and for stage I patients, chemotherapy is generally not recommended.
To summarize, chemotherapy is routinely recommended for patients with stage III; for patients with stage II, the decision of whether or not to administer chemotherapy is made on a case-by-case basis; and for patients with stage I, chemotherapy is generally not administered. In the above cases, professional doctors need to make judgment based on the condition.
So, the post-op doctor's statement that no chemo is needed is reliable .
This doc is a surgeon or oncologist, I believe. If they can say that, they must have a basis, they won't say anything, and there is no need to lie to you! You should trust the doctor's words! Don't worry too much!
Generally speaking, if the cancer invades to the submucosal layer and exceeds 1,000 micrometers, additional surgical procedures should be performed from a safety point of view, and routine chemotherapy should be administered after surgery! This would indicate that the depth of cancer invasion is shallow, and postoperative recuperation and routine rechecks would be sufficient.
The people still have certain misunderstandings about postoperative chemotherapy. Some of them think that chemotherapy is inevitable after cancer surgery, but some of them think that there is no need to do radiotherapy after surgery and tumor removal. In fact, these are not very correct.
Below is a list of patients who need chemotherapy for bowel cancer according to the Chinese Colorectal Guidelines:
I期No chemotherapy is needed after surgery, regular follow-up is sufficient
II期There are three scenarios
1. Low-risk T3N0M0,dMMR (mismatch repair functional defect), can be followed up and observed
2. Generalized T3N0M0, no risk factors and pMMR (mismatch repair function is intact) Class IA recommendation is single-agent fluorouracil chemotherapy, and Class II recommendation is observation (observation may be an option for some frail patients who are afraid to tolerate chemotherapy or who refuse chemotherapy).
3. High-risk T3N0M0/pMMR (mismatch repair functionally intact) with high-risk factors, or T4N0M0 Grade I recommendation is combination regimen chemotherapy, Grade II recommendation is single-agent fluorouracil chemotherapy (pMMR patients only) Grade III recommendation is observation
III期Postoperative adjuvant chemotherapy is recommended for resectable bowel cancer, and preoperative adjuvant chemotherapy is feasible for unresectable locally advanced bowel cancer, and surgery is almost feasible when the tumor shrinks with complete resection.
IV期For patients with advanced bowel cancer who no longer have a chance of surgery, combination chemotherapy is recommended
What are the high risk factors for patients with stage II bowel cancer?
risk factor: T4, poor histologic differentiation (grade 3/4, excluding those with MSI-H), vascular invasion, invasion of nerves, preoperative intestinal obstruction or perforation of the tumor site, positive margins or unknown condition, insufficient safe distance from the margins, and fewer than 12 lymph nodes sent for examination.
low risk factor:: Refers to MSI-H (microsatellite height instability) or dMMR (defective mismatch repair function)
common risk factor: neither high nor low risk factors
And mismatch repair protein (MMR) testing is recommended for all patients with stage II bowel cancerthat are prognostic for treatment-level prognosis. It is generally accepted that stage II patients with dMMR or MSI-H may have a better prognosis but will not benefit from adjuvant chemotherapy with single-agent 5-Fu.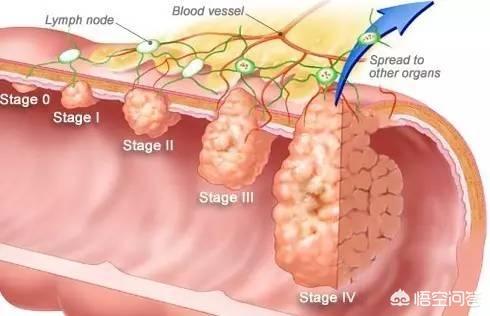
When do you start postoperative adjuvant chemotherapy?
Chemotherapy should be initiated as soon as possible after recovery from surgery. It is usually started about 3 weeks after surgery and should not be started later than 2 months after surgery, if the body permits. The total course of chemotherapy should be completed within 6 months.
In response to the questioner who is a patient with stage II bowel cancer, if there are no risk factors listed above, you may choose to observe and have regular reviews. It is recommended to review every 3 months for the first 3 years and half yearly in the 4th-5th year. After 5 years of safety, annual review is allowed.
In conclusion, I would like to say that surgery does not solve all the problems of the tumor, and whether or not you should have chemotherapy is still based on the condition and postoperative pathology.
The above is some of my clinical experience accumulated in the clinic hope to help you, I love science @ Oncology Peter Pan welcome to follow me to analyze more medical knowledge #Health Science Qualifying ##Health Science Competition ##Health Science Competition
Whether chemotherapy is given after surgery for bowel cancer depends on the patient's age, physical health, nature of tumor, degree of invasion, presence of metastasis, and whether surgical resection is bottom-cutting or not. Therefore, it cannot be generalized.
This question can only be answered by a medical professional, but a few years ago a friend of mine suffered from rectal cancer and had chemotherapy and radiotherapy, and the cancer still spread.
Friends originating from sciatica playing closed needle, the liquid did not disperse, from the inside inflammation, pus, perforation leading to anal fistula, anal fistula long time, lesions into rectal cancer, and then do proctocolectomy (not preserving the anus) rerouting surgery, postoperative chemotherapy, radiotherapy, three months after the cancer cells metastasized to the systemic lymph, six months after the person is gone.
Therefore, the doctor said that no chemotherapy is needed after the operation of bowel cancer, perhaps it is because after many years, the medical conditions are getting higher and higher, the doctors are getting more and more skillful, or perhaps the patients are in early stage and the condition is not serious, or perhaps some patients are in good physical condition, have good immunity and recover quickly, so all kinds of situations are possible.

Rather, I understand how you feel. Many of my early stage lung cancer patients also ask me, "Doc, won't you prescribe me any more drugs? Don't you prescribe me chemotherapy? What about radiotherapy? What about targeted drugs? I said, "No, your situation is very good, you don't need chemotherapy, you don't need to take medication, and you just need to check up on time.
It really needs to be explained to everyone here. Why do not you give drugs, do not allow chemotherapy, which really shows that the patient's specific situation is not bad. Radiotherapy kills not only cancer cells, but also our normal cells; targeted drugs also have certain side effects, excessive treatment will be a burden on the patient's body, which is not conducive to postoperative recovery. So if the doctor says no, then relax and follow the doctor's instructions.
However, be sure to review it on time.
It really does not mean that one can rest easy after the surgery, even if the chance of recurrence is small, there is no guarantee that it will not recur 100%; and, if a person has had a tumor, it means that genetically or physically, the person's internal environment is susceptible to tumors. Therefore, even if the tumor in this place is cured, there is no guarantee that the primary tumor will not arise again in other places. That's why some of my patients, who think they are fine after lung cancer surgery, don't have a review for two or three years, and then when they have a review again, they find out that they have other carcinoma in situ. Failure to review on time can really be a big problem.
Early stage bowel cancer can be treated with surgery. Chemotherapy is hurtful and painful, I think it is better to listen to the doctor for treatment. If you feel unreliable, you can go to a big hospital to consult other doctors and listen to their professional opinions.
Depending on your situation and the extent of the disease, you have to trust the doctor, after all, the doctor is kind-hearted
This question and answer are from the site users, does not represent the position of the site, such as infringement, please contact the administrator to delete.