Can metformin and gliclazide be used together? What are the precautions?
Pharmacist Lee answered this question from two aspects: firstly, can metformin and gliclazide be taken together to control blood glucose in patients with type II diabetes mellitus, and secondly, how do you know when to take the two medications? Is it okay to take them early in the morning after meals?
Metformin + gliclazide can be combined to control blood sugar
As we all know, metformin is the drug of choice and the basic drug for people with type 2 diabetes mellitus, and the diabetes guidelines of all countries point out that metformin should be the drug of choice for type 2 diabetes mellitus if it is not contraindicated and has been retained in the medication regimen. In addition to effectively reducing hepatic glucose output and lowering blood glucose and glycated hemoglobin protein in diabetic patients, it also has a protective effect on the cardiovascular system in diabetic patients, therefore, as a long-term medication for diabetic patients, metformin has become a core medication.
Gliclazide belongs to sulfonylureas, which are insulinotropic agents, and its main effect is to lower blood glucose by stimulating the pancreatic β-cells to secrete insulin and increase the level of insulin in the body. Gliclazide is also a kind of hypoglycemic drug that has been used for a long time, with sure hypoglycemic effect and high safety. In addition to the hypoglycemic effect, Gliclazide can also reduce the thrombosis of microvessels in the process of diabetic complications, and partially inhibit platelet adhesion and aggregation, therefore, long-term use can reduce the risk of diabetic microangiopathy and macrovascular lesions.
In terms of mechanism of action, metformin is able to improve insulin resistance and reduce hepatic glucose output; gliclazide is able to promote insulin secretion and lower blood glucose, the mechanism of action of the two drugs just complement each other, which makes it a good drug combination. A randomized double-blind parallel clinical study proved that the combination of metformin and sulfonylurea can control fasting blood glucose and glycated hemoglobin more effectively than these two drugs alone. It is important to note that when combining these two medications, be aware of the risk of hypoglycemia occurring.
When should I take metformin and gliclazide?
First of all, the metabolic characteristics of the two drugs in the body, metformin into the body, 1 ~ 2 hours to reach the peak blood concentration, its plasma half-life of 5 ~ 6 hours, so for ordinary tablets or enteric-coated tablets, can be divided into two to three times a day, ordinary tablets are recommended to be taken during meals or immediately after meals to reduce gastrointestinal irritation, enteric-coated tablets are recommended to be taken half an hour before a meal, fasting is conducive to the drug to enter the intestine more quickly. It is recommended to take it half an hour before meals, and taking it on an empty stomach will help the drug enter the intestine more quickly. In addition, metformin is also available in an extended-release formulation, which can be taken once a day and, like the regular, is recommended to be taken with or immediately after a meal.
After taking Gliclazide, it can reach the peak plasma value in 3~4 hours, and the half-life of the drug is 10~12 hours, so it is generally recommended to take it 1~2 times a day, if it is a slow-release tablets, it can be taken once a day, for the time of taking, there is no special requirement for Gliclazide, but because this drug also has the effect of causing gastrointestinal side effects, so it is more reasonable to take it after meals.
Therefore, in response to the question posed by the subject, if you are taking metformin extended-release tablets and gliclazide extended-release tablets, it is okay to take them immediately after breakfast, and in the case of other dosage forms, you can refer to the number of times and methods of dosing mentioned above.
You can.
Hello, I am glad to be here to help answer the questions in your mind. Before we start taking treatment, let's first understand the classification and range of blood glucose values, as well as what treatment options are currently available for diabetes, and what you should do to cooperate with your doctor in your treatment.
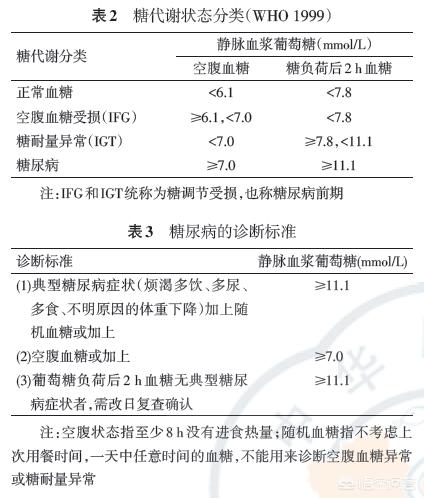
According to the classification of glucose metabolism published by the World Health Organization, normal fasting blood glucose ranges from 3.9 to 6.1 mmol/L. Fasting blood glucose values of 6.1 to 7.0 mmol/L are called pre-diabetes, and diabetes can be clearly diagnosed when fasting blood glucose exceeds 7.0 mmol/L (two or more measurements are required).
Oral hypoglycemia is currently the most accepted way, metformin, as the most widely used oral hypoglycemic agent, is recommended by all guidelines as the first-line drug for controlling hyperglycemia in patients with type 2 diabetes mellitus and as the basic drug in drug combinations. If there are no contraindications and intolerance, metformin treatment should be considered, and if the effect of single-drug treatment is not satisfactory, two- or three-combination therapy or multiple injections of insulin can be initiated. Lifestyle interventions should accompany the initiation of drug therapy for diabetes, and it is recommended to maintain a certain level of physical activity.
The main pharmacologic effect of bisphosphonates is to lower blood glucose by reducing hepatic glucose output and improving peripheral insulin resistance. Sulfonylureas promote insulin secretion, and the combination of the two classes of drugs, with their complementary mechanisms of action, provides better control of fasting glucose and glycosylated hemoglobin and reduces the risk of weight gain.
Common discomforts with metformin include gastrointestinal reactions, Metformin can be taken with a meal or immediately after a meal, and the extended-release dosage form is taken 1x/d with dinner or immediately after a meal. It is recommended to start with a small dose and gradually increase the dose, the minimum recommended dose for onset of action is 500mg/d, the maximum dose available for adults is 2550mg/d, and the optimal effective dose is 2000mg/d. Gliclazide is recommended to be taken with breakfast. Therefore, it is not a problem to take these two drugs together after breakfast.
References:
1. Chinese Medical Association Diabetes Section. Guidelines for the prevention and treatment of type 2 diabetes in China (2017 edition). Chinese Journal of Diabetes. 2018, 10(1):4-67.
2. mother YM, Ji LN, Ning G, et al. Expert consensus on the clinical application of metformin (2016 edition). Chinese Journal of Diabetes. 2016, 24(10):871-884.
3. China Expert Panel on Endocrine Related Drugs. Expert consensus on the clinical application of sulfonylureas (2016 edition). Drug Evaluation. 2017, 14(1):5-12.
The authoritative interpretation of Pharmaceutical Affairs, unauthorized reproduction, plagiarism will be punished.
The first thing that can be determined is thatYou can take these two medications together every day after breakfastThe problem is that your fasting blood glucose is still 8.0mmol/L! However, if your fasting blood glucose is still 8.0 mmol/L despite taking metformin and gliclazide, there are three problems to consider: first, poor dietary control; second, low physical activity; and third, inappropriate choice of medication or insufficient dosage of medication;
First of all, you can try to control your diet and increase the amount of exercise, in the two glucose-lowering drugs to take the same number of times and the dose of the same, with half a month as the deadline, monitor your blood sugar level, if you can ultimately control the blood sugar value of 7.0 or less, then, this shows that your medication program is still okay, if the value of the blood sugar value of 7.0 or more, you need to consider a change in your medication regimen!
In fact, it is not recommended to take sulfonylurea hypoglycemic drugs right off the bat for people with first-onset diabetes. Although this drug is powerful, its hypoglycemic effect comes at the cost of squeezing the potential of pancreatic islet cells, which doesn't do much good for pancreatic function! It is mostly used when metformin alone is not effective in controlling the condition!
Because most of the diabetic patients initially islet function damage is not very serious, insulin synthesis and secretion disorder is not too serious, at this time high blood sugar is more due to the body tissue cells to insulin sensitivity is reduced, so, at this time, we should first consider the use of Metformin, if the use of Metformin blood glucose value is still on the high side, then, we can increase the number of times and the dose of this drug, until the level of control of the blood glucose. Until the blood sugar level can be controlled! When this drug alone fails to control the condition, then we should consider adding a sulfonylurea such as gliclazide!
Metformin extended-release tablets, for example, can be taken at a maximum dose of 2,000 milligrams!
Suggestion 1: Go to the hospital to have your islet function and insulin levels measured for glucose-lowering medication selection!
Recommendation 2: Take only metformin extended-release tablets, one tablet (500 mg) once a day with dinner, and gradually increase to four tablets (2000 mg) at a time if blood glucose control is poor; if blood glucose is still uncontrolled, split the four tablets into two meals, i.e., two tablets (1000 mg) at breakfast and two tablets (1000 mg) at dinner!
Recommendation 3: If you still insist on taking metformin and gliclazide at the same time, then you should choose metformin extended-release tablets (size 500 mg) and gliclazide extended-release tablets (size 30 mg), the dosage should be as follows: one gliclazide extended-release tablets (30 mg) for breakfast and metformin extended-release tablets (500 mg) for dinner every day, and if your blood sugar is not under good control, you can increase the dosage of both of them. dose, where metformin extended-release tablets can refer to recommendation 2, and the maximum dose of gliclazide extended-release tablets can be increased to 120 mg once daily!
Note 1: Glucose-lowering drugs need to be increased gradually from a lower dose; the timing of the increase should be: when there is still no significant decrease in blood glucose level for more than two consecutive weeks!
Note 2: Controlling the amount of food you eat and increasing the amount of exercise you do is very important!
The above is purely personal opinion and is not intended as a guide to clinical use of medication, if necessary, please consult a specialist!
Metformin and gliclazide are a common combination.
Metformin is the first-line drug for diabetes mellitus, and its mechanism of action is to lower glucose by promoting the conversion of blood glucose into lactic acid by anaerobic fermentation. It can easily lead to gastrointestinal irritation, liver and kidney damage, and most importantly, lactic acid accumulation can easily trigger lactic acidosis and aggravate ketoacidosis. This is also the reason why taking biguanide must pay attention to hypoglycemia, because hypoglycemia is easy to trigger fat protein glucose isomerization, producing a large amount of lactic acid pyruvic acid and even lead to acidosis!
Gliclazide, on the other hand, works by stimulating insulin secretion, not to mention that stimulating insulin secretion accelerates pancreatic decline, and it's generally not recommended to take it for three months in a row. The biggest problem is that gliclazide can cause hypoglycemia.
What you need to know is that severe hypoglycemia causing lactic acidosis or ketoacidosis can cause you kidney failure just once! Doctors and pharmacists don't tell you about these side effects, probably because the drug is their only weapon.

Let's move on to what's going on with a fasting blood sugar of 8.
High fasting blood sugar means you have significant insulin resistance.
Four common conditions that trigger high fasting blood glucose are:1. Decrease in cell surface insulin receptors caused by prolonged and heavy consumption of sugary foods. Cells store blood glucose as fat, resulting in increased cell size and increasing difficulty in accommodating blood glucose.2. Insulin inefficiency caused by severe hyperlipidemia.3. Sumuj reaction caused by hypoglycemic stress.4. Massive secretion of multiple glucagon hormones in the body caused by stressors such as staying up all night, drinking alcohol, stress, nervousness, and negative emotions, which inhibit insulin action!
The most likely cause of fasting glucose is stress-induced insulin resistance!
Taking metformin and gliclazide will not eliminate insulin resistance, or more precisely, there is no medication that can eliminate insulin resistance, and you need to reflect on what you have triggered that triggers resistance. It must be regulated by diet and habits to be the right solution.
As a typical lifestyle disease, diabetes cannot be overly dependent on medication, and must be regulated from multiple perspectives, diet, exercise, emotion, and breathing are all very important. The most important thing is to first distinguish what the most likely triggers of their blood sugar abnormalities are, and find the root cause of the disease, so that nature can be better regulated.
Vista has been engaged in chronic disease rehabilitation guidance for 11 years, about more hypertension, diabetes, high uric acid, hyperlipidemia and other diseases of the non-pharmacological management methods are inside the Wukong Q&A. This article is Vista's 514th answer in Wukong, interested in seeing more of my Q&A.
vista specializes in non-drug conditioning and gives you all the dry stuff! Thank you for liking and following us!
Hi, as an endocrinologist I am happy to answer your question. Metformin and gliclazide are both glucose-lowering drugs, but the glucose-lowering mechanism is different. Metformin is currently used as a first-line drug for type 2 diabetes, as long as there are no contraindications can be used, it is mainly to inhibit hepatic glycogen output, increase the utilization of glucose in peripheral tissues, there is an improvement in the role of insulin resistance, in addition to its commonly used gastrointestinal response, appetite suppression, mild weight loss effect. Gliclazide is a sulfonylurea drug, the main pharmacological effect is to stimulate the pancreatic β-cell secretion of insulin, increase the level of insulin in the body and reduce blood glucose. They have complementary effects and can be used together to control blood sugar, but not meant to be taken at the same time. Gliclazide is usually taken before meals, and must be taken before breakfast and dinner for short-acting and once before breakfast for long-acting. Metformin, on the other hand, is usually taken after meals, mainly to minimize its gastrointestinal symptoms, but of course it can also be taken before or during meals. In short, gliclazide is a pro-secretory agent, taking it after meals may easily lead to hypoglycemia, and is not recommended to be taken after meals.
Thanks for the invite!
Metformin and gliclazide are two drugs that can be used in combination.
A. Metformin and gliclazide are in that class of hypoglycemic drugs?
Metformin is a biguanide glucose-lowering drug, which mainly acts on the liver to reduce glucose isomerization; it can also act on the gastrointestinal tract to delay the absorption of glucose in the gastrointestinal tract, and also increase the utilization of peripheral glucose. It is mainly used for type 2 diabetes mellitus that cannot be controlled by diet and exercise, especially obese non-insulin-dependent diabetes mellitus; it can also be used as an adjunct to insulin-dependent diabetes mellitus. It has the advantage of not easily causing hypoglycemia.
Gliclazide belongs to the sulfonylurea hypoglycemic drugs. It mainly acts on pancreatic β-cells and promotes the release of insulin from the pancreas to produce hypoglycemic effect. It is mainly used for mild and moderate type 2 diabetes mellitus with unsatisfactory dietary exercise control.
Second, can metformin be combined with gliclazide?
Through the above mechanism of action of the drug can be seen, the two drugs lowering sugar to act at different sites, can be used in combination to enhance the effect of lowering sugar, but pay attention to hypoglycemic reaction.
Third, is it possible to eat together after breakfast?
Gliclazide and metformin should be taken with breakfast; you can take the medication at the same time as your first meal, but do not take it after breakfast. Metformin is also taken twice a day, both with meals, depending on blood sugar control.

IV. Precautions
The first thing is to be careful to avoid hypoglycemia;
Contraindicated in renal disease or liver or kidney insufficiency;
Contraindicated in congestive heart failure requiring treatment;
Acidosis and diabetic ketosis are contraindicated;
Liver function, kidney function, and blood glucose should be monitored frequently while taking the medication;
In combination with anticoagulants, monitor coagulation;
Avoid excessive alcohol consumption;
Vitamin B12 supplementation is appropriate;
Discontinue metformin for 48 hours before using iodine-containing contrast media;
Check the fundus of the eye frequently;
When combined with diuretics, hormones, diphenhydramine antihypertensive drugs, niacin, and other medications, blood sugar control may be affected and hyperglycemia may occur.
However, some studies have concluded that the combination of these two did not have a better glucose-lowering effect than metformin alone.
Glucose-lowering medications are used to keep blood sugar at normal levels without hypoglycemia. These two medications can be combined, and exactly how effective they are can be gauged by monitoring your blood sugar.
First of all, from the time of taking the drug, metformin can be taken before and after meals, if there is a significant gastrointestinal reaction, it is recommended to take after meals, you can also use enteric-coated tablets to reduce gastrointestinal stimulation. Gliclazide onset of action time is more special, from the action curve, 30 minutes before meals can achieve the best effect, so take 30 minutes before meals. Secondly, fasting can only reflect the basic blood glucose situation, you need to monitor the blood glucose 2 hours after meals, through the blood glucose situation after three meals to adjust the drug dose.
Thanks, I can't answer you on this question, it's about your health. Some medicines can't be taken by anyone who is ready to take them, some before meals and some after. I suggest you still go to the hospital to check according to the doctor's method of taking, taking medication is not a joke, according to the instructions to take routine. For the sake of your health, I wish you a speedy recovery.
Dr. Duan's Q&A Online 🔑 Metformin and Gliclazide Combination for Lowering Blood Sugar 🔑
Metformin and glargine (including gliclazide) together are the most common combination for oral hypoglycemia, and many people take them this way. The most significant caveat of taking both drugs is - hypoglycemia.
Advantages of combining metformin and gliclazide for hypoglycemia:
The causes of type 2 diabetes: first, insulin resistance (that is, insulin's glucose-lowering function is not fully realized), and second, the amount of insulin is insufficient.
Metformin, which belongs to the class of biguanide glucose-lowering drugs, can enhance the insulin to play a glucose-lowering role. Gliclazide, belonging to the sulfonylurea class of insulin secretion drugs, can promote insulin secretion. The two drugs complement each other to lower blood sugar better.
Precautions for the combination of metformin and gliclazide:
(1) A common side effect of gliclazide is hypoglycemia; metformin alone does not cause hypoglycemia, but the two-drug combination increases the risk of hypoglycemia.
(2) Type 2 diabetes is a progressive disease that culminates in an impaired pancreas that rarely secretes enough insulin even when stimulated. Therefore, if the combination of the two drugs fails to control blood glucose, gliclazide must be exchanged for insulin.
(3) Switching to insulin application is recommended when acute or chronic complications occur, such as ketoacidosis, hyperglycemic hypertonic state, moderate to severe renal disease, severe liver disease, acute infection, shock, and surgery.

Dr. Duan specifically warned:
(1) When only one of the drugs is taken and blood sugar control is poor, a combination of the two drugs works better. When two drugs are taken in combination and blood sugar control is poor, gliclazide needs to be replaced with insulin.
(2) Regularly check fasting blood sugar and glycosylated hemoglobin.
(3) Dietary control and adherence to exercise are the foundation of diabetes treatment and must be adhered to with or without medication.
☞ Follow Dr. Duan for health and wellness!
Hello, thank you for your invitation, more diabetes-related knowledge, please WeChat search WeChat public number "sugar doctor said"!
Is your question understandable in two parts:
1. Is it possible to take both medications with a fasting blood sugar of 8.0?
In general, diabetes glycemic control goals need to be individualized, different ages, different complications and different concomitant diseases glycemic control goals are different, therefore, you need to understand your age, complications and other physical conditions in order to comprehensively determine whether your current medication is reasonable!
2. Can these two drugs be taken at the same time with meals?
Metformin is usually divided into two kinds, enteric-coated capsules (such as Junlida) and tablets (such as Geritol), usually enteric-coated capsules are taken before meals, and tablets are taken after meals; while gliclazide is an insulinotropic agent, usually taken before meals, and it is not recommended to be taken after meals; it can be combined with the kind of medication you take to determine your own!
This question and answer are from the site users, does not represent the position of the site, such as infringement, please contact the administrator to delete.