What exactly is mother-to-child HIV blocking?
Mother-to-child HIV blockade (MTCT) refers to the interruption of the transmission of HIV from mother to child after pregnancy in HIV-infected women through the administration of medication to pregnant women, the administration of medication to infants at birth, and artificial feeding.
Three steps to blocking:
1. Interrupting intrauterine transmission: Vertical mother-to-child transmission can occur at any time during pregnancy and accounts for 23% of mother-to-child transmission. Antiretroviral therapy should be started as soon as HIV-infected pregnant women are identified, regardless of whether or not they have had a CD4+ T-lymphocyte count and viral load test, and regardless of their test results. It is the most effective intervention that does not require discontinuation of the medication after delivery, regardless of the infant feeding method. This is because mother-to-child infections are most likely to occur during labor and delivery, and the risk spikes the closer you get to delivery, which is the most dangerous time. In short, if you can reduce the virus in the mother's body with anti-HIV medication, the child is less likely to become infected.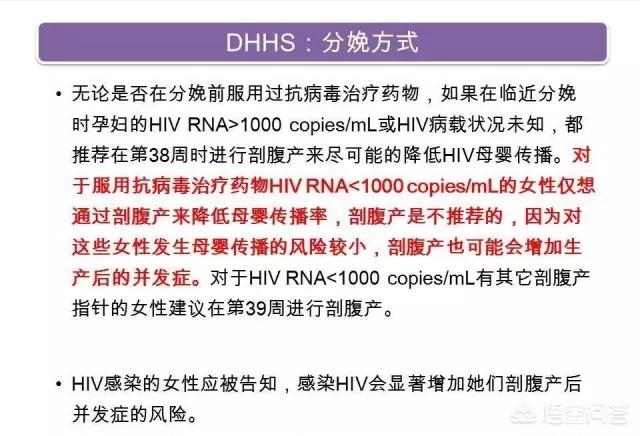
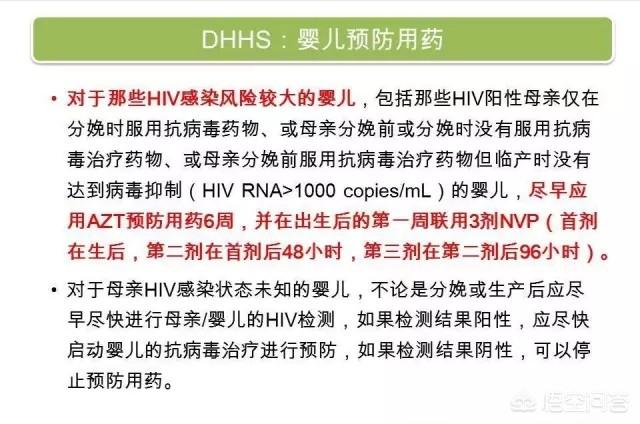
2. Blocking transmission during delivery: It is currently believed that the risk of vertical transmission of HIV during delivery is the greatest, and that the fetus will be infected through contact with the mother's blood and cervico-vaginal secretions that contain the virus, which accounts for 65% of mother-to-child transmission. Cesarean section is not recommended for women who have started antiretroviral therapy in early or mid-pregnancy, are taking medication regularly, have no clinical symptoms of AIDS, or have a viral load of <1000 cp/ml in late pregnancy, or are in labor. For pregnant women with viral load >1000 cp/ml and without antiretroviral therapy, elective cesarean delivery can effectively prevent mother-to-child transmission of HIV. Labor should be closely observed and actively managed during delivery, and injurious operations that may increase the risk of mother-to-child transmission should be avoided as much as possible, including perineal circumcision, artificial rupture of membranes, the use of fetal head attractors or forceps, and intrauterine fetal scalp monitoring. After birth, newborns should be cleaned promptly with running warm water, and nasal and oral mucosa should be cleaned with ear washing ball to shorten the time that newborns come into contact with the mother's blood, amniotic fluid and secretions. The cleaning process should be done gently to avoid damaging the skin and mucous membranes.
 3. Artificial feeding: HIV in breast milk can infect newborns through their mouth or gastrointestinal tract, accounting for 12% of mother-to-child transmission. For HIV-infected women who cannot breastfeed their babies themselves, it is necessary to choose good quality and safe breast milk substitutes and to use artificial feeding to avoid the transmission of HIV through breast milk in the postpartum period. For those who choose to breastfeed, adequate counseling should be provided, emphasizing the need for the mother or baby to continue to take antiretroviral medication during the feeding period, and instructing on proper exclusive breastfeeding practices and breast care. They are advised that breastfeeding should ideally last no longer than six months, while actively creating conditions for an early change to artificial feeding.
3. Artificial feeding: HIV in breast milk can infect newborns through their mouth or gastrointestinal tract, accounting for 12% of mother-to-child transmission. For HIV-infected women who cannot breastfeed their babies themselves, it is necessary to choose good quality and safe breast milk substitutes and to use artificial feeding to avoid the transmission of HIV through breast milk in the postpartum period. For those who choose to breastfeed, adequate counseling should be provided, emphasizing the need for the mother or baby to continue to take antiretroviral medication during the feeding period, and instructing on proper exclusive breastfeeding practices and breast care. They are advised that breastfeeding should ideally last no longer than six months, while actively creating conditions for an early change to artificial feeding.
Medical treatment measures that minimize the chances of vertical transmission of HIV from mother to child through a series of services such as antiretroviral treatment, safe delivery, and guidance on artificial feeding. The implementation of mother-to-child interruption can reduce the chance of mother-to-child transmission of HIV from 30-40% to 2-5%.
This question and answer are from the site users, does not represent the position of the site, such as infringement, please contact the administrator to delete.